2436
Hyperpolarized 129Xe MR functional imaging to monitor the response of the human lungs after segmental lipopolysaccharide challenge1Institute of Diagnostic and Interventional Radiology, Hannover Medical School, Hannover, Germany, 2Biomedical Research in Endstage and Obstructive Lung Disease Hannover (BREATH), German Center for Lung Research (DZL), Hannover, Germany, 3Department of Clinical Airway Research, Fraunhofer Institute for Toxicology and Experimental Medicine, Hannover, Germany, 4Department of Radiology and Medical Imaging, University of Virginia, Charlottesville, VA, United States, 5Department of Radiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Hyperpolarized 129Xe MRI has been shown to be sensitive to inflammatory changes after lung provocation by lipopolysaccharide (LPS) in an animal model. The purpose of this work was to investigate feasibility of monitoring the response of the human lungs after segmental LPS challenge using 129Xe MRI. Dissolved-phase imaging and chemical shift saturation recovery were employed to assess inflammatory changes and to compare MRI results with inflammatory cell counts from bronchoalveolar lavage. Both MRI methods show a significant reduction of the 129Xe in red blood cells and lung tissue ratio in the affected region but no significant correlations with inflammatory cell counts.
Introduction
Hyperpolarized 129Xe MRI has been proven to be a highly sensitive probe for regional lung function and previous work has shown sensitivity of 129Xe MRI-derived parameters for inflammatory changes after lung provocation by lipopolysaccharide (LPS) in an animal model [1]. The purpose of this work was to investigate the feasibility of monitoring changes in regional lung function parameters after segmental LPS challenge using hyperpolarized 129Xe MRI in humans, to compare results derived from imaging and localized spectroscopy [2,3] and to compare MRI results with inflammatory cell counts from bronchoalveolar lavage.Methods
The institutional ethics review board approved this study and thirteen healthy volunteers were recruited. Imaging was performed at 1.5 T (Avanto, Siemens) using a birdcage transmit and 16-channel phased-array receive coil (Rapid Biomedical). Hyperpolarization of 129Xe was achieved by spin-exchange optical pumping using a commercially available polarizer (Model 9800, Polarean).
Hyperpolarized 129Xe MRI sessions were performed one week before (baseline) and 24 h after segmental LPS challenge (provocation). Bronchoalveolar lavage was performed in the challenged segment and inflammatory cells (neutrophils, macrophages, lymphocytes and monocytes) were assessed. The MR protocol included dissolved-phase imaging (DPI) [2] and chemical shift saturation recovery (CSSR), for which the volunteers inhaled 1 L and 0.5 L hyperpolarized 129Xe, respectively, and a variable amount of air. The air volume was chosen such that a breathing position of 1/3 forced vital capacity for DPI and total lung capacity for CSSR, respectively, were achieved. High-resolution 3D ventilation imaging was performed during the same breath-hold as the aforementioned sequences.
Both for dissolved-phase imaging and CSSR spectroscopy, 129Xe signals were separated into gaseous 129Xe (GP), 129Xe in aqueous solution (tissue and blood plasma, TP), and in red blood cells (RBC). The CSSR sequence employed two phase-encoding steps in head-foot direction.
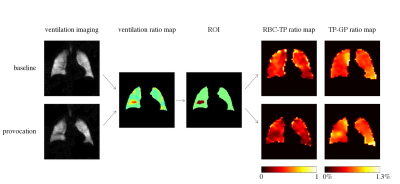
A ratio map of ventilation after provocation compared to baseline imaging was derived. Using a region-growing algorithm, regions of mildly decreased ventilation in the challenged segments were automatically identified and used as regions of interest (ROIs) for further data analysis. Spectral localization of CSSR data was achieved using the described ROIs and coil sensitivities obtained from ventilation imaging by application of Spectral Localization Achieved by Sensitivity Heterogeneity (SPLASH) [3,4]. The Patz model [5] was used for assessment of lung microstructural parameters using CSSR data.
Results
Ten volunteers successfully completed the study protocol and were included for data analysis. Figure 1 shows exemplary ventilation images from one volunteer along with the corresponding ventilation ratio map, the ROI used for data analysis and dissolved-phase imaging data. The average RBC-TP ratio in the ROI applied to co-registered dissolved-phase imaging data was significantly lower (two-sided Wilcoxon signed-rank test, p = 0.004), whereas the average TP-GP ratio was significantly elevated (p = 0.049) after provocation, as shown in figure 2. Localized CSSR also exhibited significant reduction of RBC-TP averaged at a fixed delay time of 50 ms (p = 0.014). There was a significant correlation of RBC-TP in the ROI derived from DPI and CSSR (Pearson’s ϱ = 0.452, p = 0.045).
A trend for elevated surface-to-volume ratio derived from the TP resonance was visible, which was not statistically significant (p = 0.106). Unlike in reference [1], no change in septal wall thickness derived from the TP resonance (TPWT) was observed (p = 0.557).
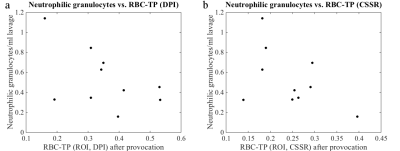
No significant correlation of imaging-derived parameters with the amount of inflammatory cells was found after LPS challenge. However, there was a trend of an inverse correlation of RBC-TP and number of neutrophilic granulocytes (Pearson’s ϱ = –0.508, p = 0.134 for imaging data and ϱ = –0.492, p = 0.149 for CSSR data), see figure 3.
Discussion
Data from both dissolved-phase imaging and localized CSSR independently exhibit a reduction of the RBC-TP ratio after segmental LPS challenge, strengthening the validity of the findings. The authors ascribe this effect to pulmonary edema, which impedes gas uptake to RBC by interstitial thickening.
The existence of pulmonary edema would suggest an increase in TPWT, which was not observed. However, TPWT must be seen as an average wall thickness and the effect of wall thickening might be masked by the signal contribution of fast-saturating regions. This effect can be expected to be increased by the affected region’s underventilation.
Conclusion
Lung areas with segmental LPS challenge show a local reduction in the gas-uptake parameter RBC-TP, likely due to pulmonary edema causing expansion of the interstitial space in the lung parenchyma. Hyperpolarized 129Xe dissolved-phase imaging and localized CSSR may have added value to lavage fluid analysis.Acknowledgements
This research was funded by the German Center for Lung Research (DZL).References
[1] Månsson et al., Magn Reson Med 2003;50:1170–1179
[2] Qing et al., NMR Biomed 2014;27:1490–1501
[3] Kern et al., Proc Intl Soc Magn Reson Med 2017;4917
[4] An et al., Magn Reson Med 2011;66:1–10
[5] Patz et al., New J Phys 2011;13
Figures