2435
Measuring the Impact of PEEP on Pulmonary Gas Transport Using Hyperpolarized Xenon-129 Dissolved-Phase MRI1Radiology, University of Pennsylvania, Philadelphia, PA, United States
Synopsis
Higher positive end-expiratory pressure (PEEP) during mechanical ventilation can result in improved oxygenation, but it can also give rise to ventilator-induced lung injury. In this work, we used a rabbit model to evaluate the sensitivity of a hyperpolarized xenon-129 MRI technique that allows a comprehensive assessment of the pulmonary gas-transport by the entire lung for monitoring the impact of PEEP on lung function. We observed that increased PEEP resulted in a large decrease in pulmonary gas transport that is most likely linked to a lengthened pulmonary transit time.
Purpose
The optimization of positive end-expiratory pressure (PEEP) during mechanical ventilation—in the management of acute respiratory distress syndrome (ARDS), for instance—continues to present a clinical challenge. While higher PEEP can result in improved oxygenation, it can also give rise to ventilator-induced lung injury1,2. In this work, we propose the use of a hyperpolarized xenon-129 (HXe) MRI technique that allows for the comprehensive assessment of pulmonary gas-transport by the entire lung as a tool for monitoring the impact of PEEP on lung function. We evaluated the sensitivity of this method in a rabbit model at several PEEP settings.Methods
Imaging experiments were performed in a sedated New Zealand rabbit (approx. 4.5 kg). The animal was ventilated with room air until imaging began, at which point the gas mix was switched to 20% oxygen and 80% HXe for two breaths (6 ml/kg tidal volume). Imaging was performed at end inspiration of the second breath. All studies were approved by the Institutional Animal Care and Use Committee.
MR imaging was conducted using a 2D-projection gradient-echo sequence that employed a non-selective 900-μs Gaussian RF excitation pulse centered 3,530 Hz downfield from the gas-phase resonance. The large frequency difference between the two phases, combined with a sufficiently small acquisition bandwidth, allowed us to simultaneously image HXe in the pulmonary air spaces and dissolved in the lung tissue side-by-side3. The following sequence parameters were used: matrix size 36×80; TR/TE 100/2.7 ms; flip angle 25°; FOV 230 mm; receiver bandwidth 110 Hz/pixel. The change of the HXe signal in the left ventricle was calculated as the ratio of the average signal in a region of interest in the heart at PEEP 1, 2.5 or 4 cm, respectively, and the signal at zero PEEP. All MR studies were performed at 1.5T (Avanto; Siemens), using a custom xenon-129 transmit/receive birdcage coil (Stark Contrast, Erlangen, Germany). Enriched xenon gas (87% xenon-129) was polarized using a prototype commercial system (XeBox-E10, Xemed LLC, Durham, NH).
Results and Discussion
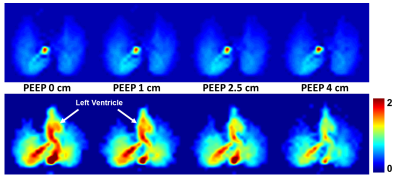
Figure 1 shows the normalized HXe ventilation images (top row) and the simultaneously-acquired maps of HXe dissolved in the lung parenchyma and blood (bottom row) in a healthy rabbit as a function of the applied PEEP. While the ventilation pattern remained almost unchanged, we observed a marked decrease in the signal of the dissolved xenon throughout the lung. The xenon signal in the left ventricle, which is indicative of the overall gas-transport volume of the lung, dropped by 5%, 17% and 30% for a PEEP of 1 cm, 2.5 cm and 4 cm, respectively.
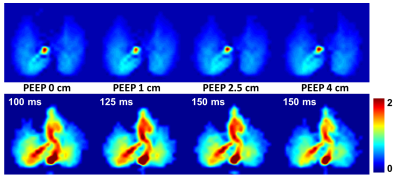
As illustrated by Fig. 2, the drop in dissolved-phase signal in the heart can be compensated for by increasing the TR of the measurement. As the intrapulmonary pressure rises, the pulmonary vasculature gets compressed and even partially collapsed, resulting in an overall increase of the transit time required for pulmonary circulation. We hypothesize that the relative change in TR that restores the heart signal to its value at zero PEEP mirrors this lengthening of circulatory transit time in the lung.
Conclusion
In this work, we demonstrated the use of HXe MRI to measure the reduction in pulmonary gas transport caused by increased PEEP settings during mechanical ventilation. Our results suggest that HXe MRI could become an important tool for improving our understanding of the impact of PEEP on overall lung function, as well as for minimizing the risk of ventilator-induced lung injuries.Acknowledgements
Supported by NIH grants R01 EB015767 and R01 HL129805.References
[1] Cereda et al. Quantitative imaging of alveolar recruitment with hyperpolarized gas MRI during mechanical ventilation. J Appl Physiol 2011;110:499-511.
[2] Sahetya et al. Setting Positive End-Expiratory Pressure in Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 2017;195:1429-1438.
[3] Mugler et al. Simultaneous magnetic resonance imaging of ventilation distribution and gas uptake in the human lung using hyperpolarized xenon-129. Proc Natl Acad Sci USA 2010;107(50):21707-21712.
Figures