2180
Evaluation of dynamic DCE-MRI of the temporomandibular joint1The Czech Academy of Sciences, Institute of Scientific Instruments, Brno, Czech Republic, 2Department of Clinical Engineering, Haukeland University Hospital, Bergen, Norway, 3Department of Radiology and Nuclear Medicine, St Olav Hospital HF, Trondheim, Norway, 4Department of Circulation and Medical imaging, Norwegian University of Science and Technology, Faculty of Medicine, Trondheim, Norway, 5Department of Radiology, University Hospital of North Norway, Tromsø, Norway, 6Dept of Radiology, Haukeland University Hospital, Bergen, Norway, 7Dept of Clinical Sciences, University of Bergen, Bergen, Norway, 8Department of Radiology, Haukeland University Hospital, Bergen, Norway, 9Dept Physics and Technology, University of Bergen, Bergen, Norway
Synopsis
The feasibility of DCE-MRI as a tool to investigate perfusion of temporomandibular joints (TMJs) in case of Juvenile Idiopathic Arthritis (JIA) in children is investigated. The hypothesis in this current study is that inflammation is associated with increased vascularity and is the origin of experienced pain. Contrary to previous studies, high temporal resolution (~4s) dynamic DCE-MRI using advanced pharmacokinetic models are for the first time applied when imaging the TMJ in JIA children aged 6-15. Results of deconvolution show that there is a difference in perfusion parameters between affected and unaffected patients, especially when permeability-surface area product (PS) and blood plasma flow (Fp) parameters are combined.
Introduction
Juvenile Idiopathic Arthritis (JIA) is a heterogeneous condition including all forms of chronic arthritis of unknown origin and affects around 1-2 children in 1000 under the age of 16. There is increasing evidence that many, if not most, children with JIA will have a chronic disease with ongoing activity into adulthood, and that the temporomandibular joints (TMJs) are more frequently involved than previously believed. However, the reported incidences are highly inconsistent due to difference in methodology (MRI is considered gold standard), thus hampering the effective use of therapeutic interventions in early childhood. The hypothesis in the current study is that inflammation is associated with increased vascularity and is the origin of experienced pain. Contrary to previous studies, high temporal resolution (~4s) dynamic DCE-MRI is for the first time applied when imaging the TMJ in JIA children aged 6-15. To investigate the proposed methodology, five different pharmacokinetic models are compared in terms of characterization of lateral differences in a subset of the investigated children, i.e. in about 10% of 100 clinical examinations performed so far. Estimated parameters were compared to clinical information.
Methods
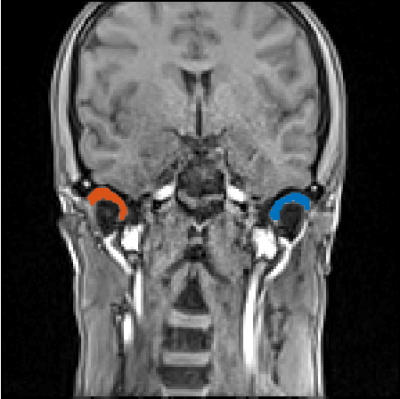
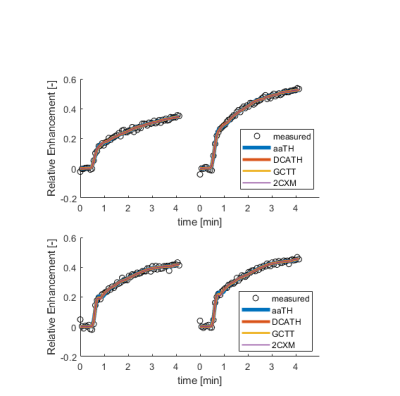
An extended imaging protocol was performed on a 3Tesla Siemens Skyra using a 64-channel head coil, A dynamic T1-weighted DCE-MRI sequence (FLASH-3D TR/TE/FA/=4ms/1ms/9°, matrix 160x160x16, 60 volumes in time) was measured. The gadolinium-based contrast-agent, Dotarem, was injected using a power injector (injection speed 5mL/s, 10 seconds after start of data acquisition). All imaging was performed in accordance with ethical guidelines. Three dimensional (3D) volumes of interest (VOI) covering synovial TMJ were drawn manually to identify the right (R) and left joint (L), respectively (Fig.1). These VOIs were selected based on consensus between three radiologists, and always on the 5th precontrast volume in each individual. The signal changes in the voxels that were completely within the VOIs were averaged and relative enhancements curves, i.e. (signal-baseline)/baseline, were estimated. In house developed MATLAB(2017b) software tool was used for the subsequent data analysis. Arterial input functions (AIFs) were selected semi-automatically by selecting in each individual a large region that included the large brain feeding arteries and then automatically selecting the voxels with the highest signal peak within this region. Deconvolution was performed using four different advanced pharmacokinetic models (aaTH1,2, DCATH3, GCTT3,4 and 2CXM implemented as constrained GCTT). These models are able to separate vascular and parenchymal phase of signal enhancement and so estimate a full set of parameters (Fig.2.). Patient datasets were split into two groups; unaffected (4 females, 3 males, age 9-15) and affected (4 females, age 6-14). Ratios of parametric estimates were computed between left (L) and right (R) TMJ in each individual. Boxplots showing relative errors vs. pharmacokinetic model and each patient group were constructed for all parameters. Then two parameters with the biggest differences among groups are put together to improve robustness. Finally data of boxplots were tested using the Wilcoxon’s rank sum test for significance of difference in medians and whether median of unaffected group is lower compared to affected group. The model with lowest p-value was selected with respect to number of free parameters
Results
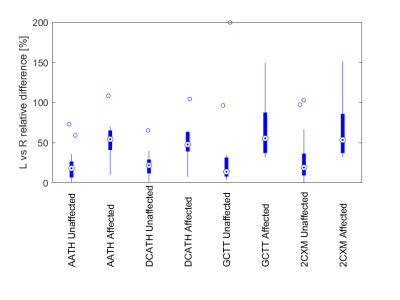
All models interpolated the measured data with no substantial residue (Fig.3.). The relative differences of affected children compared to unaffected children were systematically higher for Fp and PS. Relative differences of these two were combined together in a single boxplot (Fig.4.). Differences of medians were tested using the Wilcoxon signed rank test (Fig.5.). Statistical test confirmed that unaffected group has lower median of relative differences compared to affected group. Lowest p-value was observed in case of GCTT model.
Discussion
The proposed approach to evaluate affection of TMJ is feasible using DCE-MRI. The affected group had higher variance and higher medians indicative of increase uptake (flow) as indicative inflammation. Boxplots show that relative differences in perfusion parameters are higher in case of disease, however this can also be caused by uncertainties of fitting algorithm. Thus, GCTT and DCATH should not be preferred, because they have one additional free parameter compared to aaTH, 2CXM and are probably more susceptible to noise. From two remaining models i.e. aaTH and 2CXM, the aaTH performed better compared to 2CXM, because of lower p-value 0.0077 and much narrower boxplots indicating higher numeric stability.Conclusion
Results show that DCE-MRI of TMJ is feasible. In following stage all of 100 patients will be included. With more dataset in database it would be possible to reveal pattern how disease affects perfusion parameters. Adding reference region will make it possible to localize affected side of TMJ and uncover both side inflamation, which is not possible at this stage. Deconvolution using the aaTH model will be preffered.Acknowledgements
The research was supported by by grants from the the Czech Science Foundation (grant no. 16-13830S) and by the MEYS CR (LO1212).References
[1] St Lawrence KS, Lee TY. 1998. An adiabatic approximation to the tissue homogeneity model for water exchange in the brain: I. Theoretical derivation. J. Cereb. Blood Flow Metab. 18(12):1365–77.
[2] Bartos M. et al. 2014. The precision of DCE-MRI using the tissue homogeneity model with continuous formulation of the perfusion parameters. Magn. Reson. Imaging. 32(5):505–13.
[3] Koh TS. et al. 2001. The inclusion of capillary distribution in the adiabatic tissue homogeneity model of blood flow. Phys. Med. Biol. 46(5):1519–38.
[4] Schabel MC. 2012. A unified impulse response model for DCE-MRI. Magn. Reson. Med. 68(5):1632–46.
[5] Koh TS, Bisdas S, Koh DM, Thng CH. 2011. Fundamentals of tracer kinetics for dynamic contrast-enhanced MRI. J. Magn. Reson. Imaging. 34(6):1262–76.
Figures