2141
Importance of early spectral variations during 36 months of longitudinal follow MRI and MRS in 90 patients treated glioblastomas1CHU et Université Amiens, Picardie, France, Amiens, France, Metropolitan, 2TsinghuaUniversity, Beijing, Chine, Beijing, China, 3Université de Rouen, France, Rouen, France, Metropolitan
Synopsis
MRS allows non-invasive follow-up of treated glioblastomas tumors. There is a large variability, but repetition and modelisation of spectroscopic measurements during longitudinal follow-up could allow us to diminish it and to improve prognostic evaluation especially in long survivors and patients with proliferation relapses. Studying the relationship between MRS measures, segmentation and perfusion parameters could lead to better understanding of tumoral processes and of therapeutic response, especially with regard to chemotherapy, radiotherapy and antiangiogenic molecules and in the future oxidative stress and hypoxia modulators.
Introduction
to better understand glioblastomas tumor metabolism and post chemotherapy, radiotherapy and antiangiogenic variations and to determine cerebral variation in MRS measures of metabolites and spectral profiles during a 36 months longitudinal follow-up in 90 patients with glioblastomas tumors with different resection percentage, hyperperfusion and contrast enhancement initially and treated with STUPP protocol and antiangiogenic.Subjects and Methods
Over 90 patients all biopsied and all treated by surgery and STUPP protocol, 53 underwent antiangiogenic therapy and more than 400 exams were done MRI: Sagittal T1, axial FLAIR, diffusion, coronal T2, 3D T1 and late axial T1 after gadolinium. MRS: 1H, single voxel (6 to 12 cm3), PRESS with multiple TEs on a 3 T or 1,5 T (GEMS). Data processing: SA/GE, JMRUI yielding amplitudes, areas, ratios (Cho/Cr, CH2/Cr, NAA/Cr and Lac/Cr), and relative concentrations. Statistical analysis of longitudinal MRI, perfusion and spectroscopic data (every 2 months over 36 months).Results
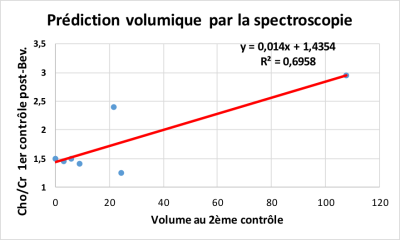
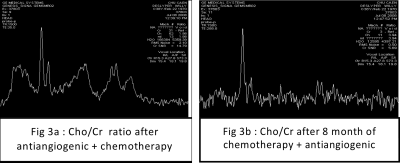
quantitative studies in MRI with multi-spectral segmentation and tissular classification are ongoing. Spectroscopic profiles improve under STUPP protocol, then worsen with increases in Choline/N-Acetyl-Aspartate (Cho/NAA), Cho/Cr and CH2 lipids/Cr and lactate/Cr ratios, and decreases in NAA/Cr. After STUPP, chemotherapy and antiangiogenic therapies tumoral volumes (necrosis and contrast enhancement), in MRI, change between two exams while spectroscopic profiles and ratios do change more. MRS could, in fact with proliferation who persists then increases or reappear (Cho/Cr increase), be earlier and more sensitive than MRI and could be predictive of clinical worsening even the hyperperfusion or the enhancement disappear. The water and creatine are quite stable, especially in the contralateral side, which could justify using them for some other ratios to quickly detect spectroscopic variations. Effect of TE on measurements: Concentration of NAA always has higher estimation on the short TE while lactate often has higher estimation on the 288 ms TE. Spectroscopic and metabolic changes often come well before clinical deterioration and sometimes before improvement. Therefore, MRS could be more sensitive and could detect changes earlier than MRI and sometimes is predictive. The analysis of spectral profiles from long survivors is interesting.Discussion/Conclusion
Temozolomide and Avastin were well tolerated. MRI changed (especially CE and Necrosis) in T1 for most of the patients but MRS changed more with variable ratio of mI/Cr, increase Cho/Cr, Glx/Cr, lactate/Cr, CH2 lipids/Cr and decrease NAA/Cr at baseline. We observed a decrease in Cho/Cr ratio and hyperperfusion and contrast enhancement decrease for patients whose clinical condition improved and inverse results for those whose conditions deteriorated. MRS allows non-invasive follow-up of treated glioblastomas tumors. There is a large variability, but repetition and modelisation of spectroscopic measurements during longitudinal follow-up could allow us to diminish it and to improve prognostic evaluation especially in long survivors and patients with proliferation relapses.
Studying the relationship between MRS measures, segmentation and perfusion parameters could lead to better understanding of tumoral processes and of therapeutic response, especially with regard to chemotherapy, radiotherapy and antiangiogenic molecules and in the future oxidative stress and hypoxia modulators.
Acknowledgements
No acknowledgement found.References
Hattingen, et al2007 ; Dou W, et al2007 ; Artzi M, et al. 2014 ; Stadlbauer A, et al.2015Figures
Fig 1a: Glioblastoma’s MRI. The quantitative MRI studies with a multi-spectral tissue segmentation and classification are being
Fig 1b: Glioblastoma jMRUI processed spectra, TE=35ms and TE=144ms
Glioblastoma spectrum on SCI-MRS-LAB
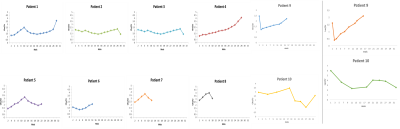
a: Example of ratio monitoring of Cho/Cr Areas (TE = 144 ms) over 32 months in 10 patients with glioblastomas. Cho/Cr ratios are variable with a tendency to improve at the beginning of treatment with sometimes, aggravation even under antiangiogenic when they become multifocal.
b: Figure 5 : Example of Lactate/Cr ratio monitoring (at TE=288ms or 144ms) over 32 months in 2 patients with glioblastoma.