2139
Quality of Life, Neurocognitive Function and T2 FLAIR Hyperintensity Volume in Stable Grade II and III Glioma Patients1Radiology and Biomedical Imaging, UCSF, San Francisco, CA, United States, 2Neurological Surgery, UCSF, San Francisco, CA, United States
Synopsis
Quality of life and neurocognitive function are important clinical outcome measures for patients with lower grade glioma. In this pilot study, we performed neurocognitive testing and quality of life assessments in radiologically and clinically stable grade II and III glioma patients who were not receiving active treatment. We found novel associations between standard clinical assessments and neuroimaging metrics at pre-surgical and follow-up timepoints. Further characterizing the longitudinal relationship between structural and functional neuroimaging, neurocognition and quality of life will better allow clinicians to proactively intervene to help patients in future.
INTRODUCTION
Improved treatments for patients with gliomas (primary brain tumors arising from glial cells) have increased survival, yet many patients continue to suffer from neurocognitive deficits and poor quality of life in their remaining years,1,2. This includes lower grade (WHO grade II-III) glioma patients who are radiologically and clinically stable and who often have residual T2 FLAIR abnormalities on standard clinical imaging. In this pilot study, we performed neurocognitive testing and quality of life assessments in this subset of patients on the same day as their clinical follow-up MRI to determine the relationship between pre-surgical and residual T2 FLAIR hyperintensity, neurocognitive function and quality of life.METHODS
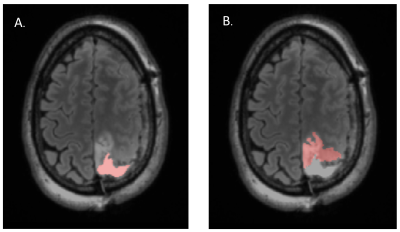
Clinical, standard of care MRI examinations were performed on 19 patients (see Table 1 for population characteristics) on a 3T GE scanner with an 8 or 32 channel head coil and included T2-weighted 3D FLAIR and FSE and T1-weighted IRSPGR images with and without gadolinium contrast. We assessed MRIs acquired on the same day as the neurocognitive evaluation as well as immediately prior to the previous surgery. Residual and pre-surgical T2 FLAIR hyperintensity regions of interest (ROIs) were created using in-house software and manually edited. In addition, volumes of the T2 FLAIR abnormality, cavity from any prior surgery and cysts if present were combined to quantify lesion burden (Figure 1).
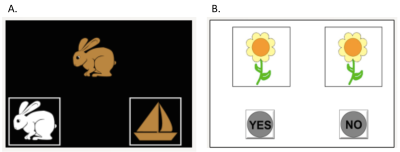
Standardized neurocognitive testing was performed in approximately 45 minutes with the NIH Toolbox Cognitive Domain modules (nihtoolbox.org) displayed on an iPad (Figure 2). The neurocognitive battery included the Picture Sequence Memory Test (spatial and episodic memory), Pattern Comparison Processing Speed Test, Dimensional Change Card Sort Test (attention and executive function), Flanker Inhibitory Control and Attention Test, Picture Vocabulary Test (language comprehension and vocabulary), Oral Reading Recognition Test (reading and speech) and List Sorting Working Memory Test. To control for age-related cognitive decline, we used age-normalized scores in our analyses. Quality of life was evaluated with the Functional Assessment of Cancer Therapy-Brain (FACT-BR). We also acquired patient demographic information, treatment history, tumor location, and histologic and molecular tumor characteristics. Multiple regression was used to assess the relationship between clinical characteristics, T2 FLAIR hyperintensity volumes and neurocognitive and quality of life scores.
RESULTS
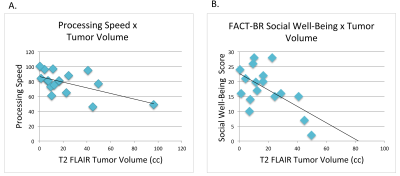
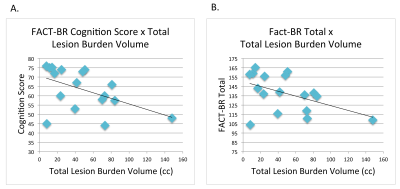
Pre-surgical lesion burden ROI volume was significantly related to the self-reported FACT-BR cognition subscale and total quality of life score, with larger volumes corresponding to poorer cognitive ability and quality of life (Figure 3a). Larger residual T2 FLAIR hyperintensity volume on the day of neurocognitive testing was significantly associated with worse processing speed (lower score on the Pattern Comparison Processing Speed Test) and worse social well-being on the FACT-BR (Figure 3b). Patients as a group were impaired on processing speed, with a mean score of more than 2SD below age-matched healthy controls. In addition, chemotherapy was associated with worse attention and executive function (lower score on the Dimensional Change Card Sort Test); patients with a history of radiation reported worse social well-being (FACT-BR subscale); and patients with IDH-mutated astrocytomas had higher total cognitive scores than patients with oligodendrogliomas.DISCUSSION
The correlation between larger lesion burden on MRI prior to surgery and self-reported impairments in cognition and quality of life at follow-up underscores the potential vulnerability of this population and highlights the need for proactive interventions. The association between residual T2 FLAIR hyperintensity volume at the time of neurocognitive testing and deficits in processing speed and interpersonal relationships should inspire future studies.CONCLUSION
This pilot study found novel associations between standard clinical assessments and neuroimaging metrics at pre-surgical and follow-up timepoints and demonstrates the feasibiity of using the NIH Toolbox and the FACT-BR to evaluate neurocognitive function and quality of life in grade II and III gliomoa patients at the time of their follow-up visit. Serial collection of this data is underway. Further characterizing the longitudinal relationship between structural and functional neuroimaging, neurocognition and quality of life will better allow clinicians to proactively intervene to help patients in future.Acknowledgements
This research was supported by the American Cancer Society. The authors would also like to thank the patients who made this study possible.References
1. Boele FW, Klein M, Reijneveld JC, et al. Symptom management and quality of life in glioma patients. CNS Oncol. 2014 Jan;3(1):37-47. 2. Talacchi A, Santini B, Savazzi S, et al. Cognitive effects of tumour and surgical treatment in glioma patients. J Neurooncol. 2011 Jul;103(3):541-9.Figures