2084
Increased Glutamate in Anterior Cingulate Cortex in Crohn’s Disease Patients with Abdominal Pain Revealed by Proton MR Spectroscopy1Zhejiang Chinese Medical University, Hangzhou, China, 2Radiology, The First Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China, 3Gastroenterology, The First Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, China, 4MR research, GE Healthcare, Shanghai, China
Synopsis
Based on Brain-gut axis, the study used proton magnetic resonance (MR) spectroscopy, a noninvasive detection to reveal the alteration of metabolites in bilateral perigenual anterior cingulate cortex (pgACC) in patients with Crohn’s disease (CD) with abdominal pain. Twenty nine CD patients (cases with/without abdominal pain, 16/13) and 20 healthy controls were recruited for comparison. The pain CD group showed increased Glutamate (Glu) levels in bilateral pgACC, which might provide new insight into the neural mechanism of the disease in abdominal pain processing.
Purpose:
There have been increasing occurrences of Crohn’s disease (CD) in recent years, especially in developing countries.1 Abdominal pain is the main clinical manifestation of CD, which causes patient discomfort and significantly decrease quality of life. The pathogenesis remains yet fully understood. Based on Brain-gut Axis, study have found patients with CD and with pain involved abnormal activities of specific brain regions in the processing of visceral pain in the central nervous system.2 The study aimed to determinate the alternations of metabolites in specific brain region of CD patients with abdominal pain by using proton magnetic resonance spectroscopy (MRS) and the relationship with the presence of abdominal pain to further explore the neural mechanism.Methods:
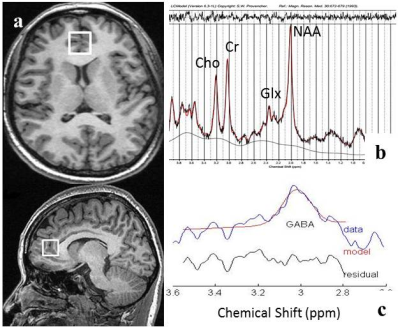
The study protocol was approved by the Ethics Committee of our hospital. All participants provided written informed consent. Sixteen CD patients with abdominal pain (average age 28.56±7.10 years, ranged 18-38 years, 6 females and 10 males) and 13 CD patients without abdominal pain (average age 39.69±13.83 years, ranged 23-67 years, 5 females and 8 males), and 20 healthy controls (average age 29.35±7.59 years, ranged 24-50 years, 8 females and 12 males) were recruited in this study. The clinical scores included Visual Analogue Scale (VAS) of pain, Hospital Anxiety and Depression (HAD) Scale, and Crohn's Disease Activity Index (CDAI) were evaluated before MR scan. The metabolites of specific brain region were measured by PRESS (point resolved spectroscopy) of MRS on a 3T MR scanner (Discovery 750, GE Healthcare, Milwaukee, WI). We selected the bilateral perigenual anterior cingulate cortex (pgACC) as the region of interest (ROI) of MRS. In the middle stage of experiments; nine CD patients and eight healthy controls (HCs) were applied the MEGA-PRESS (Mescher-Garwood point resolved spectroscopy) in the same ROI to reveal the γ-aminobutyric acid (GABA) concentration. The metabolites were quantitatively analyzed by LCmodel (linear combination of model, Provencher, 1993) and Gannet (GABA-MRS analysis tool). A two independent sample T test and one-way analysis of variance (ANOVA) were performed in statistical analysis. Spearman correlation was conducted to examine the relationship between the metabolites levels and clinical scores.Results:
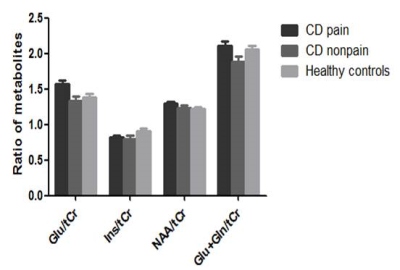
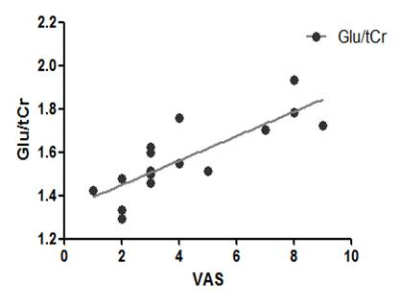
There were no significant difference in gender among the pain and non-pain CD group and the HC group (all p > 0.05). The results quantitatively analyzed by LCmodel indicated that the CD patients with abdominal pain have statistically higher levels of Glutamate (Glu)/(creatine + phosphocreatine, total creatine, tCr) than that of CD patients without abdominal pain, and controls (p=0.003, p=0.009, respectively) in pgACC. Moreover, within pain CD group, Glu levels positively relationship with the subjective level of pain experienced by participants (r= 0.857, P=0.000). However, the results indicated that there were no statistical differences in (Glu + glutamine, Gln)/ tCr, N-acetylaspartate (NAA)/tCr and myoinositol (Ins)/tCr among three groups (all p > 0.05). Meanwhile, the results quantitatively analyzed by Gannet indicated that CD patients have significantly lower levels of GABA+/tCr (p=0.002) than controls. To some extent, CDAI had the trend of negative correlation with (GABA+)/tCr levels (p=0.088, r=-0.6).Discussion and Conclusion:
CD patients with abdominal pain had a different metabolite status in bilateral pgACC. These altered concentrations of metabolites were correlated with visceral perception, which suggested that the CD patients with abdominal pain processing the pain in central nervous system involved with neurochemical metabolites. Unbalance of Glu and GABA levels may play a key role in pain processing in patients with CD with abdominal pain. Further study requires more subjects and needs to measure other brain regions rather than pgACC.Acknowledgements
No acknowledgement found.References
1. Ng SC, Bernstein CN, Vatn MH, et al. Geographical variability and environmental risk factors in inflammatory bowel disease. Gut. 2013;62: 630-649.
2. Bao CH, Liu P, Liu HR, et al. Differences in regional homogeneity between patients with Crohn’s disease with and without abdominal pain revealed by resting-state functional magnetic resonance imaging. Pain. 2016;157: 1037-1044.
Figures