2070
Cerebral Vascular Reactivity and Cognitive Decline in Healthy and in Early Stages of Pathological Aging.1Neuroradiology, CHU Grenoble, Grenoble, France, 2Grenoble Institute of Neuroscience, Grenoble, France, 3Neurology, CMRR Grenoble, CHU Grenoble, Grenoble, France, 4IRMAGE, Grenoble, France, 5CNRS, LPNC, Chambéry, France, 6CHU Grenoble, Grenoble, France, 7CNRS, LPNC, Grenoble, France
Synopsis
Cerebral blood flow (CBF) and cerebral vascular reactivity (CVR) decrease with age and might affect cognitive functions. In this study, we investigated their correlation with cognitive abilities during normal and pathological aging.
We performed neuropsychological assessments on thirty-four participants: 13 healthy-young, 10 healthy-old and 11 impaired-old. We measured CBF and CVR using hypercapnia and Arterial Spin Labeling imaging.
Regarding the impaired-old, we found specific decrease in executive functions, short-term and working memory. Significant correlations were found between CVR and cognitive scores. Global CBF correlated only with age.
Unlike CBF, CVR reduction was specifically associated with cognitive decline during aging.
INTRODUCTION
Normal aging is associated with vascular changes, which affect basal perfusion expressed as cerebral blood flow (CBF) and functional changes of perfusion such as cerebral vascular reactivity (CVR). However, in pathological aging CBF and CVR decrease is more important and shows regional specificities. Previous studies suggested the possible hemodynamical origin of neurodegenerative disease and its impact on cognitive abilities. Moreover, at early stages of pathological aging, cognitive difficulties are difficult to distinguish from the effect of normal aging. Nevertheless, previous studies showed that subjective cognitive complaints seemed to be an early sign of pathological cognitive decline. Therefore, we investigated CBF and CVR changes and their correlation with different cognitive domains, during normal aging and at the subjective-cognitive-complaint stage of pathological aging.METHODS
We performed neuropsychological assessments on 34 participants: 13 healthy young adults (44.1±9.5yo), 10 healthy older adults, without cognitive complaint (72.1±5.7yo), 11 older adults, with cognitive complaint (73.4±7.9yo). We tested cognitive functions, including attention, short-term and working memories, executive functions and language. We measured basal CBF and CVR elicited by hypercapnic challenge (7%CO2) using pseudo-continuous ASL (3T Achieva TX, Philip, post-label delay=1525 ms; voxel=3x3x6 mm3; 20 slices; TE 12 ms; TR=4s for a total of 180 control and tag volumes acquired in 12 min during block-designed hypercapnia). Individual end-tidal CO2 pressure (mmHg) was simultaneously recorded and further used as a physiological regressor to conduct linear regression analysis. Post-processing was performed using AMIGOv0.9, an in-house software (Python3.6, Matlab8.6, SPM12), giving whole-brain and regional basal CBF and CVR. We performed Kruskal-Wallis to test the effect of AGE on: neuropsychological scores, CBF, and CVR values. We performed post-hoc comparisons, in case of significance. Furthermore, we conducted Spearman's rank correlation analysis on AGE, Neuropsychological scores, CBF and CVR values, within several brain regions.RESULTS
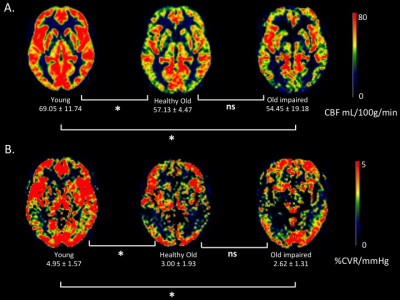
We found a significant AGE effect on CBF and CVR. However, there was no significant difference between the older adults groups. See Figure 1. Furthermore, we found regional differences in CBF and CVR between the three groups. They were lower in posterior regions for adults with cognitive complaint.
We also found a decrease in attention and inhibition within older participants. Older adults with cognitive complaint showed specific decrease in global cognitive functioning, executive functions, short-term and working memory.
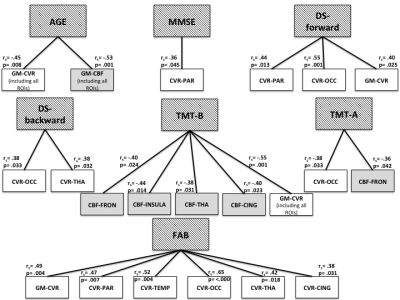
Finally, correlation analyses revealed a strong relationship between cognitive outcomes and CVR within several brain regions, while global CBF correlated only with AGE. Regional CBF, however, correlated with attention and inhibition processes within anterior regions. See Figure 2.
DISCUSSION
Attention and inhibition were affected by normal aging, which is in line with the General Slowing Theory. Older participants with cognitive complaints showed global cognitive functioning, executive functions, short term and working memory decline, in accordance with the Frontal Theory of cognitive aging. Our results confirmed that subjective cognitive complaints were predictive of objective cognitive difficulties.
Our results should be taken with caution due to the modest number of participants. However, other studies failed to show significant difference in CBF between healthy older adults and patients with MCI or AD. Hence, we may assume that at early stages of neurodegenerative disease, CBF drop would reflect the normal aging effect.
However, the patterns of CBF and CVR decline in healthy aging and at early stages of pathological aging were heterogeneous, which confirms that CVR impairment is independent from CBF decline with aging.
The most interesting finding is that global CBF correlated negatively only with age. Regional CBF correlated with attention and inhibition, which decline naturally with age, while CVR correlated with all cognitive scores, except for language.
CONCLUSION
Overall, our results show that CBF reduction takes place naturally with age without affecting dramatically cognitive functions. On the other hand, CVR decline is more likely to be associated with cognitive difficulties 1. Furthermore, we found a consistency between regional CVR reductions and the neurofunctional hypotheses underlying each region of interest. Although we need to take our results with caution, they support the idea that vascular dysfunction could lead to cognitive deficits in neurodegenerative disease 2,3. Moreover, a review of 113 articles published during this last decade highlighted the evidence of brain-vessels contractility dysfunction in AD, and claimed that despite the variability between studies, CVR is clearly compromised in neurodegenerative disease and should definitely be considered as a diagnosis tool and/or as a preventive therapeutic target 4.Acknowledgements
We thank IRMaGe MRI/Neurophysiology facility, which was partly funded by the French program “Investissement d’Avenir” run by the "Agence Nationale pour la Recherche"; grant "Infrastructure d’avenir en Biologie Santé" - ANR-11-INBS-0006.
This work was funded by Région Rhône-Alpes.
References
1. Richiardi J, Monsch AU, Haas T, et al. Altered cerebrovascular reactivity velocity in mild cognitive impairment and Alzheimer’s disease. Neurobiol Aging. 2015;36(1):33-41. doi:10.1016/j.neurobiolaging.2014.07.020.
2. Montagne A, Nation DA, Pa J, Sweeney MD, Toga AW, Zlokovic BV. Brain imaging of neurovascular dysfunction in Alzheimer’s disease. Acta Neuropathol (Berl). 2016;131(5):687-707. doi:10.1007/s00401-016-1570-0.
3. Dichgans M, Leys D. Vascular Cognitive Impairment. Circ Res. 2017;120(3):573-591. doi:10.1161/CIRCRESAHA.116.308426.
4. Glodzik L, Randall C, Rusinek H, de Leon MJ. Cerebrovascular reactivity to carbon dioxide in Alzheimer’s disease. A review. J Alzheimers Dis JAD. 2013;35(3):427-440. doi:10.3233/JAD-122011.
Figures