2031
Nilvadipine slows progression of white matter hyperintensities in Alzheimer’s disease1Radboudumc Alzheimer Center, Radboud university medical center, Donders Institute for Brain, Cognition and Behavior, Nijmegen, Netherlands, 2Trinity College Institute of Neuroscience, Trinity College Dublin, Dublin, Ireland
Synopsis
Cerebrovascular disease, such as presence of white matter hyperintensities (WMH), contributes to Alzheimer’s disease (AD) pathology and progression. The antihypertensive nilvadipine may reduce WMH progression by reducing amyloid-induced vasoconstriction and improving cerebral perfusion. Here we show that in patients with mild to moderate AD, nilvadipine slows the increase of WMH after 6 months, but not after 18 months, when correcting for baseline WMH. This contradicts the view that reducing blood pressure in an elderly dementia population leads to progression of white matter damage and instead seems to have a beneficial effect on WMH.
Background
Alzheimer’s disease is characterized by beta amyloid plaques and neurofibrillary tau tangles in the brain, but in recent years the contribution of vascular disease to AD pathology and progression has become more clear. For instance, white matter hyperintensities (WMH), visualized on MR imaging and reflecting cerebral small vessel disease, are elevated in AD and those at risk for AD [1]. The calcium-channel-blocker nilvadipine has previously been shown to impact on both amyloid beta clearance and on vascular dysfunction, and this antihypertensive has been proposed as a disease modifying therapy in AD [2]. Nilvadipine may reduce WMH progression by reducing amyloid-induced vasoconstriction and improving cerebral perfusion. However, concern exists among clinicians that lowering blood pressure (BP) in the elderly population could actually lead to hypoperfusion and increased white matter damage [3]. The aim of the current study is to investigate the effect of nilvadipine on WMH in patients with mild to moderate AD after 6 and 18 months.Methods
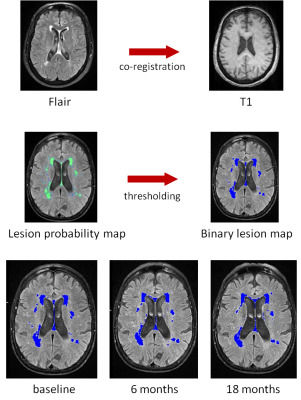
A total of 47 patients with mild to moderate AD (Mini-Mental State Examination [MMSE]≥12) were included from a multicenter double-blind randomized controlled trial (NILVAD) on the effect of the calcium-channel-blocker nilvadipine. BP and MRI measurements were performed at baseline, after 6 months and after 18 months use of nilvadipine (n=25) or placebo (n=22). This included a T1 image (magnetization prepared rapid acquisition gradient echo, MPRAGE; TR=2300 ms, TE=4.71 ms, TI=1100 ms, voxel size=1 mm isotropic) and a fluid attenuated inversion recovery sequence (FLAIR; TR=12000 ms , TE= 121 ms, TI=2880 ms , voxel size=0.7x0.7x3 mm), both at 3T. WMH were segmented on the FLAIR images by the lesion prediction algorithm [4] using the corresponding T1 images as reference images, as implemented in the LST toolbox version 2.0.15 for SPM12. WMH volume at each time point was extracted from binary lesion probability maps (threshold 0.5) and used in subsequent statistical analyses. Linear regression analysis was performed to test the effect of treatment (nilvadipine or placebo) on WMH volume progression corrected for baseline WMH volume.Results
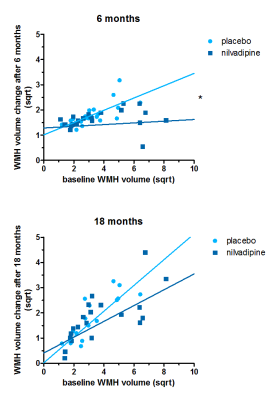
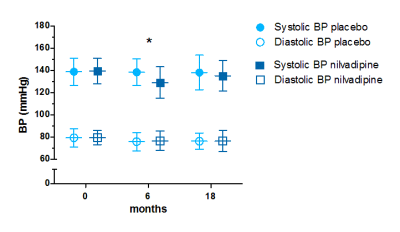
The mean MMSE score of this patient population was 16.8 (SD=3.0), mean age was 73.5 years (SD =5.8), and 18 subjects were men. Systolic BP was lower at 6 months (t(44)=-2.026, p=0.049; mean±SD mmHg nilvadipine: 129±14; placebo: 138±17), but not at 18 months (t(43)=-0.684, p=0.497; nilvadipine: 135±14; placebo: 138±15), in the group receiving nilvadipine than in the placebo group. No differences were detected in diastolic BP (all p>0.05). Square root transformations were applied to WMH volume values to obtain normally distributed data. Here, we report back-transformed estimates and confidence intervals (CI) for ease of interpretation. Baseline lesion volume, significantly predicted WMH lesion volume change after both 6 and 18 months (both p<0.001). When adding the interaction between treatment and baseline WMH volume to the model for WMH volume change after 6 months, we observed a significant interaction effect (b [95% CI] baseline WMH volume: 0.06 [0.02-0.13], p<0.001; treatment: 0.24 [0.00-0.99], p=0.069; treatment*baseline WMH volume: -0.04 [-0.12--0.01], p=0.005). This shows that in the group receiving nilvadipine, the change in WMH volume after 6 months was less than expected based on lesion volume at baseline. There was no significant interaction for change in lesion volume after 18 months (b [95% CI] baseline WMH volume: 0.25 [0.08-0.51], p<0.001; treatment: 0.13 [0.35-1.77], p=0.460; treatment*baseline WMH volume: -0.02 (-0.18-0.01], p=0.213).Conclusion
In patients with mild to moderate AD, nilvadipine slows the increase of WMH after 6 months, but not after 18 months, when correcting for baseline WMH. In addition, blood pressure showed a similar effect with lower systolic BP in subjects receiving nilvadipine, only at 6 months. This contradicts the view that reducing BP in an elderly dementia population leads to progression of white matter damage and instead seems to have a beneficial effect on WMH. Nilvadipine may temporarily reduce progression of white matter lesions, however without a long term effect on lesion volume. Whether this is driven by improved cerebral perfusion will be further investigated.Acknowledgements
This study was funded by the EU Seventh Framework Programme (grant number 279093), the Alzheimer’s Drug Discovery Foundation (20121210) and Alzheimer Nederland (WE09201503).References
1. Brickman, A.M., Contemplating Alzheimer's Disease and the Contribution of White Matter Hyperintensities. Current Neurology and Neuroscience Reports, 2013. 13(12): p. 9.
2. Lawlor, B., et al., NILVAD protocol: a European multicentre double-blind placebo-controlled trial of nilvadipine in mild-to-moderate Alzheimer's disease. BMJ Open, 2014. 4(10): p. e006364.
3. Suter, O.C., et al., Cerebral Hypoperfusion Generates Cortical Watershed Microinfarcts in Alzheimer Disease. Stroke, 2002. 33(8): p. 1986-1992.
4. Schmidt, P., Bayesian inference for structured additive regression models for large-scale problems with applications to medical imaging. 2017.
Figures