1978
Gadolinium retention in the brain – an MRI relaxometry study comparing linear and macrocyclic types of gadolinium based contrast agents1Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden, 2Department of Radiology, Karolinska University Hospital, Stockholm, Sweden
Synopsis
Gadolinium contrast agents (GBCAs) have been shown to be retained in the brain after multiple linear GBCA administrations. We aimed to quantitatively investigate T1 in relation to linear and macrocyclic GBCA-administrations in DN and GP by relaxometry. 80 MS patients who had received different types of GBCAs, were consecutively recruited. This study, in line with previous studies using semi-quantitatively methods, showed that exposure of GBCA leads to shorter T1 relaxation using linear GBCA in comparison to patients who had received macrocyclic types of GBCA, as well as patients without GBCA exposure and healthy controls.
Purpose
Gadolinium retention in the brain after administrations of gadolinium-based contrast agents (GBCA) has been demonstrated, predominantly in the dentate nucleus (DN) and globus pallidus (GP). This retention is associated with lasting high signal intensity on T1-weighted MRI and has been consistently shown for linear GBCAs.1–3 It is debated if the more chemically stable macrocyclic GBCAs lead to in vivo detectable T1 alterations.4 The commonly used semi-quantitative approaches of measuring T1 changes via signal intensity ratios may, however, have limited sensitivity. We therefore aimed to investigate T1 changes in relation to linear and macrocyclic GBCA-administrations in DN and GP by quantitative T1-relaxometry in MS patients.Materials and Methods
Study population:
We consecutively included 91 MS patients who performed a brain MRI scan between January and June 2015 at Karolinska University Hospital, Huddinge, Stockholm, Sweden in the study. Additionally, 21 age- and gender-matched healthy controls were enrolled. The local Ethics review board approved the study and written informed consent was obtained from all participants.
Image Acquisition:
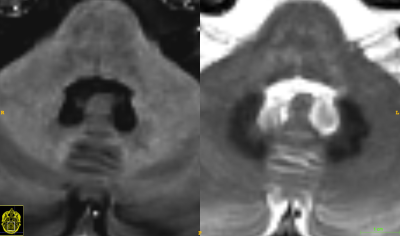
All imaging was performed on the same 3.0 T Siemens Trio MRI scanner (Siemens, Erlangen, Germany). In addition to the standard brain MRI protocol for MS, a time-efficient saturation recovery turbo spin echo sequence was used for multi-parametric relaxometry.(5) SyMRI (v. 7.2RC, Synthetic MR, Linköping, Sweden) was used to calculate the longitudinal (T1) and transversal (T2) relaxation rates, as well as PD. Radiological evaluation A resident in radiology (Y.F.) manually drew regions of interest (ROIs) blinded to all clinical information in SyMRI. Based on previous publications,2,6–8 the DN and GP were chosen as structures to place ROIs. The quantitative sequence can also generate any arbitrary spin-echo based contrast, why inherently aligned synthetic T2-weighted images were chosen to easily identify the DN and T1-weighted images to identify the GP, exemplified in Figure 1. To study the reliability of the method, the inter-rater agreement with a senior neuroradiologist (J.M.) was studied on a random subsample of 20 patients.
Clinical information:
The patients’ charts were reviewed to extract information on GBCA administrations, disease duration, disease subtype, disease modifying therapy, neuropsychological test results and expanded disability status scale (EDSS) scores.
Statistics:
SPSS version 22.00 was used for the statistical analyses. Shapiro-wilk test was used to determine if the data were normally distributed. Measures of the right and left structures were averaged. Unpaired t-test was used to compare groups. Multiple linear regression analyses were used to investigate associations between the number of received GBCA-administrations (independent variable) and the mean relaxation rates (dependent variable) in DN and GP. In as second step, associations between available neuropsychological test-scores (dependent variable), performed within a year from the MR-scan in 27 patients, and T1-relaxation rate (independent variable) were similarly evaluated with linear regression. The Intra-class Correlation Coefficient (ICC) was used in the reliability analyses between the main rater (Y.F.) and a second rater (J.M.).
Results
GBCA-administrations and T1-relaxation rates:
All T1-relaxation values for the different groups were normally distributed. The interrater ICC was 0.77 for DN and 0.73 for GP.
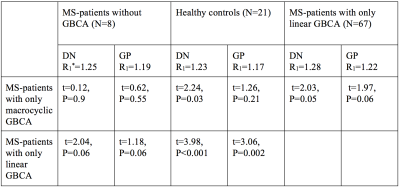
Table 1 shows the comparisons between the different groups.
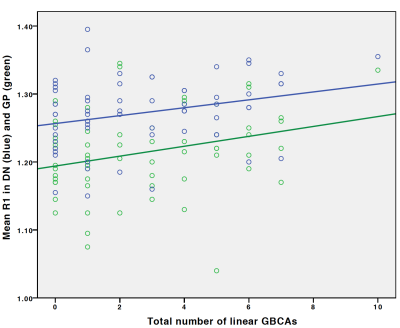
Multiple
linear regression showed that higher number of administered linear GBCA was
associated with shorter T1 relaxation rates in DN and GP (β=0.32,
P=0.006 and β=0.29, P=0.020). These results remained significant after
correction for the MS disease duration (β=0.34, P=0.005 and β=0.28, P=0.030). Figure 2 illustrates the associations between the number of GBCAs and T1-relaxation rates.
No significant associations were found between T1-relaxation rates and cognitive (information processing speed and phonologic verbal fluency) or physical outcome (EDSS).
Discussion
Here, we applied a quantitative sequence to study possible Gadolinium retention. We found that patients only receiving linear types of GBCA have a shorter relaxation rates in comparison with patients who received the macrocyclic type gadoterate meglumine. Contrary to our previously published study9 no associations with cognitive outcomes were found. By applying this quantitative approach, we avoided limitations of previously used semi-quantitative methods may have been inflicted by several risks for confounders, such as diversity of both MR-parameters and equipments (especially over a longitudinal time frame), and non-standardisation of how the ratios are measured. The use of relaxometry enables a standardized measurement method with good reproducibility.10Conclusion
Administrations of multiple linear GBCAs is associated with shorter T1-relaxation rates in GP and DN.Acknowledgements
We would like to thank the participants for making this study possible and the MRI staff at Karolinska University Hospital for their commitment. This research was supported by the Stockholm City Council and Karolinska Institutet (ALF 20120213 and 20150166). Dr. Granberg was supported by the Swedish Society for Medical Research.References
1. Kanda T, Ishii K, Kawaguchi H, et al. High signal intensity in the dentate nucleus and globus pallidus on unenhanced T1-weighted MR images: relationship with increasing cumulative dose of a gadolinium-based contrast material. Radiology 2014;270:834–41.
2. Quattrocchi CC, Mallio CA, Errante Y, et al. Gadodiamide and Dentate Nucleus T1 Hyperintensity in Patients With Meningioma Evaluated by Multiple Follow-Up Contrast-Enhanced Magnetic Resonance Examinations With No Systemic Interval Therapy. Invest Radiol 2015;50:470–2.
3. Kanda T, Oba H, Toyoda K, et al. Brain gadolinium deposition after administration of gadolinium-based contrast agents. Jpn J Radiol 2016;34:3–9.
4. Kuno H, Jara H, Buch K, et al. Global and Regional Brain Assessment with Quantitative MR Imaging in Patients with Prior Exposure to Linear Gadolinium-based Contrast Agents. Radiology 2017;283:195–204.
5. Warntjes JBM, Leinhard OD, West J, et al. Rapid magnetic resonance quantification on the brain: Optimization for clinical usage. Magn Reson Med 2008;60:320–9.
6. Errante Y, Cirimele V, Mallio CA, et al. Progressive increase of T1 signal intensity of the dentate nucleus on unenhanced magnetic resonance images is associated with cumulative doses of intravenously administered gadodiamide in patients with normal renal function, suggesting dechelation. Invest Radiol 2014;49:685–90.
7. McDonald RJ, McDonald JS, Kallmes DF, et al. Intracranial Gadolinium Deposition after Contrast-enhanced MR Imaging. Radiology 2015;275:772–82.
8. Radbruch A, Weberling LD, Kieslich PJ, et al. Gadolinium retention in the dentate nucleus and globus pallidus is dependent on the class of contrast agent. Radiology 2015;275:783–91.
9. Forslin Y, Shams S, Hashim F, et al. Retention of Gadolinium-Based Contrast Agents in Multiple Sclerosis: Retrospective Analysis of an 18-Year Longitudinal Study. AJNR Am J Neuroradiol 2017;38:1311–6.
10. Granberg T, Uppman M, Hashim F, et al. Clinical Feasibility of Synthetic MRI in Multiple Sclerosis: A Diagnostic and Volumetric Validation Study. AJNR Am J Neuroradiol 2016;37:1023–9.
Figures