1969
Three-dimensional fast spin echo with extended echo train acquisition (3D-FSE-Cube) integrate with two point water-fat separation Dixon methods (Flex): comparison with three-dimensional fast spin echo Cube in lachrymal drainage system imaging1department of radiology, Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, wu han, China
Synopsis
The normal membranous lacrimal passage and tear fluid play a very essential role in protecting and lubricating the ocular surface. An ideal lacrimal imaging is very for clinical therapy stratage. The MRI combine fluid is noninvasive and efficient. This study compared the image quality on 3D-FSE-Cube MRD and 3D-FSE-Cube-Flex MRD. The results demonstrated both of the technique has its own advantage. The mutual complementation of each other can fulfill the thorough application of MRI for qualitative images.
Introduction & Purpose:
The normal membranous lacrimal passage and tear fluid play a very essential role in protecting and lubricating the ocular surface. A clarity and exact lacrimal image information to the clinician for effective therapeutic plan is indispensable. The routine imaging modality such as the axial and coronal TWI and T2WI just provide very limited information for its thick slices. The MRD with administration of contrast media or saline solutions increase the risk of iatrogenic trauma. Previous study used 3D-FRFSE MRD and 3D-FSE-Cube MRD1-3. Nevertheless, hydrographic technique provide “all or nothing” images and failed to delineate the soft tissue structures surrounding the LDS. 3D-FSE-Cube showed hypointense cracks blended with a hyperintense lachrymal sac and/or NLD. The Cube-Flex uses a 3D-FSE acquisition and a two-point fat-water separation method to obtain high-resolution 3D images4. We postulate it may address the deficiency of 3D-FSE-Cube in some extent. our mainly purpose is to compare 3D-FSE-Cube MRD with 3D-FSE-Cube- Flex MRD on volunteers for the technical quality and the visibility of lacrimal drainage system (LDS)Methods:
21 normal volunteers underwent 3D-FSE-Cube MRD and 3D-FSE-Cube-Flex MRD at 3.0 T after topical administration of compound sodium chloride eye drops. Two board-certified radiologists studied and assessed quantitative and qualitative metrics for the images of lacrimal drainage system from each participant in a blinded fashion. The signal-to-noise ratio (SNR) of filling fluid and the contrast-to-noise ratio (CNR) of fluid-turbinate between sequences were compared separately by employing appropriate statistical methods. The two sequences were also compared for overall image quality, sharpness, artifacts, visualization of overall anatomy structures and visibility of five individual ductal segments of LDS.Results:
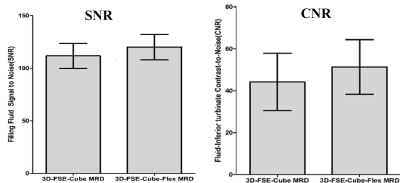
3D-FSE-Cube-Flex MRD demonstrated statistically improvement in overall image quality, visualization of anatomic structures and artifact (p<0.001, respectively) but equivalent sharpness (p=0.157) in comparison with those on 3D-FSE-Cube MRD sequence. 3D-FSE-Cube MRD showed lower filling fluid SNR and fluid-inferior turbinate CNR than 3D-FSE-Cube-Flex MRD (P<0.001, respectively). In comparison with 3D-FSE-Cube-Flex MRD, 3D-FSE-Cube MRD produced excellent canaliculi visibility (superior canaliculi, P=0.003, common canaliculus, P=0.033 and inferior canaliculi, P<0.001) but worse ductal visibility in lower lacrimal drainage (lacrimal sac, P=0.001 and nasolacrimal duct, P<0.001). There was no difference from each other for total segments of per LDS (P=0.068).Discussion:
the 3D-FSE-Cube –Flex technique is a challenge as well as a integration of the 3D-FSE volumetric acquisition with the modified two-point Dixon water-fat separation with flexible echo times.it implement a phase-correction algorithm based on a region-growing scheme but without usual constraints on the echo times 5. This single-pass mode accelerates and increases SNR efficiency of Flex applications, yielding a final water-only image and a final fat-only image with improved SNR and CNR performance. 3D-FSE-Cube-Flex MRD showed better overall image quality and anatomical visualization, which may related to the clean background, robust water-fat suppression and less artifacts. The longer repetition time, shorter echo spacing brought higher subjective rating scores of superior LDSs on 3D-FSE-Cube MRD.Conclusion:
3D-FSE-Cube-Flex MRD coupled with a two-point fat-water separation based on FTED technique is a promising technique over the 3D-FSE-Cube MRD with routine fat suppression, providing homogeneous fat suppression, less artifact and noticeable improvements in image quality of lower LDSs. Nevertheless, 3D-FSE-Cube MRD provide conspicuity display of the upper LDSs. The mutual complementation may replace the currently used 3D hydrographic MRD combined with other routine sequence, simplify the work- flow and improve the examine efficiency.Acknowledgements
This study has received funding by the National Natural Science Foundation of China (No.81301192 and No.81771793).References
1.Zhang J, Chen L, Wang QX, et al. Diagnostic performance of the three-dimensional fast spin echo-Cube sequence in comparison with a conventional imaging protocol in evaluation of the lachrymal drainage system. Eur Radiol. 2015;25(3):635-43.
2. Jing Z, Lang C, Qiu-Xia W, et al. High-spatial-resolution isotropic three-dimensional fast-recovery fast spin-echo magnetic resonance dacryocystography combined with topical administration of sterile saline solution. Eur J Radiol. 2013;82(9):1546-51.
3. Zhang J, Chen L, Wang QX, et al. Isotropic three-dimensional fast spin-echo Cube magnetic resonance dacryocystography: comparison with the three-dimensional fast-recovery fast spin-echo technique. Neuroradiology. 2015;57(4):357-65.
4.Del Grande F, Santini F, Herzka DA, et al. Fat-suppression techniques for 3-T MR imaging of the musculoskeletal system. Radiographics : a review publication of the Radiological Society of North America, Inc. 2014;34(1):217-33.
5.Eggers H, Brendel B, Duijndam A, Herigault G. Dual-echo Dixon imaging with flexible choice of echo times. Magnetic resonance in medicine. 2011;65(1):96-107.
Figures

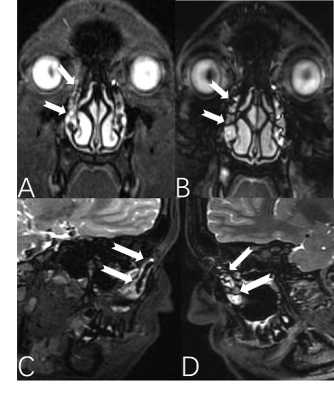
This picture show the qualitative assessment, comparison between 3D-FSE-Cube-Flex MRD and 3D-FSE-Cube MRD for ratings of artifact, sharpness, overall image quality and visualization of anatomical structures.
Flex is short for 3D-FSE-Cube-Flex MRD, Cube is short for 3D-FSE-Cube.
A two-tailed paired-sample Wilcoxon signed-rank test was utilized to compare and analyze the difference in the above quality metric. P<0.01 is significant.