1962
Diagnostic Performance of Short MR-neurography Protocol for Brachial Plexus Injuries1Radiology, Siriraj Hospital, Mahidol University, Bangkok, Thailand, 2Orthopedic Surgery, Siriraj Hospital, Mahidol University, Bangkok, Thailand
Synopsis
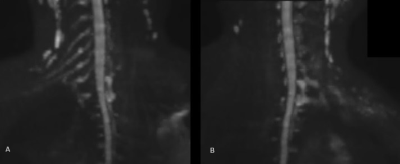
The purposes of this study were to optimize the protocol of brachial plexus MRN for brachial plexus injuries, and to study the diagnostic performance of the protocol, using clinical contexts as the reference standard. Twenty-one patients with brachial plexus injury were performed brachial plexus MRN (T2-weighted image-high resolution, mDIXON and diffusion weighted image) before conventional myelography. The diagnostic yield of T2-weighted image-high resolution was comparable to conventional myelography. The combination of T2-weighted image-high resolution and mDIXON had the highest diagnostic yield and recommended for the evaluation of brachial plexus injuries.
Background
Conventional myelography has long been used in the assessment of preganglionic root injuries. MR neurography (MRN) has recently been introduced to evaluate the proximal and distal parts of the brachial plexus. The new MRN techniques were reported to have excellent image quality and acceptable scan times by using the available coil for head/neck MR.
Purposes
To optimize the protocol of brachial plexus MRN for brachial plexus injuries, and to study the diagnostic performance of the protocol, using clinical contexts as the reference standard.Materials and methods
There were 21 patients with brachial plexus injury who were scheduled for conventional myelography. A brachial plexus MRN (T2-weighted image-high resolution, mDIXON and diffusion weighted image) was done prior to a conventional myelography on the same day. The results of the conventional myelography and the MR imaging were recorded and compared, with the clinical contexts as the reference standard. The sensitivities, specificities, positive predictive values, negative predictive values, and accuracies were calculated.Results
The accuracy, sensitivity, specificity, false positive and false negative of the conventional myelography were 69.52%, 73.61%, 60.61%, 19.70% and 48.72%, respectively; and 72.00%, 78.26%, 58.06%, 19.40% and 45.45% for T2-weighted image-high resolution, respectively. The diagnostic yield of T2-weighted image-high resolution was comparable to conventional myelography. Consequently, T2-weighted image-high resolution could be used to replace conventional myelography to diagnose preganglionic brachial plexus injuries. The accuracy, sensitivity, specificity, false positive and false negative predictive values of the combination of T2-weighted image-high resolution and mDIXON were 78.00%, 97.10%, 35.48%, 22.99% and 15.38%, respectively. The combination of T2-weighted image-high resolution and mDIXON had the highest diagnostic yield.Discussion
Most Thai patients with brachial plexus injuries are male and of a younger age because the injuries commonly occur in motor vehicle accidents, as has been reported in multiple studies1-3. Brachial plexus injuries are classified into three categories: preganglionic lesions, postganglionic lesions, and a combination of both4. The accurate diagnosis of brachial plexus injuries before surgery remains challenging. Many methods are used to evaluate the injury pattern, including physical examination, a nerve conduction study, electromyography, conventional myelography, CT myelography, and MRI. However, none of those methods is considered the reference standard5. For the evaluation of preganglionic root injuries, conventional myelography is the diagnostic tool currently used by our institute. However, it is an invasive procedure, and it takes considerably longer to perform than an MRI study. D. Somashekar et al. found that a high-resolution MRI had a similar sensitivity to CT myelography when evaluating neonatal brachial plexus palsy6. According to our results, T2-weighted image-high resolution was also comparable to conventional myelography in terms of its accuracy, sensitivity, specificity, and false positive and false negative values. In addition, T2-weighted image-high resolution is noninvasive and needs a noticeably shorter performance time (approximately 13 minutes) than conventional myelography (approximately 90-120 minutes). Furthermore, the patients are not exposed to the contrast medium, have no risk of iodine contrast allergy, and do not suffer from any side effects or radiation exposure. Therefore, we suggest that T2-weighted image-high resolution replace conventional myelography for the diagnosis of brachial plexus injuries. Conventional myelography and T2-weighted image-high resolution demonstrate preganglionic injuries, whereas mDIXON and diffusion weighted image detect postganglionic injuries. In our study, mDIXON had a slightly higher diagnostic yield than diffusion weighted image in the diagnosis of postganglionic brachial plexus injuries. In addition, mDIXON can provide accurate, indirect signs of root avulsion injuries, namely, the regional denervation of muscle changes which are seen as muscle atrophy, or a high T2 signal change, consistent with the article by A. Chhabra et al7. Therefore, mDIXON may have more benefits than diffusion weighted image in the detection of postganglionic lesions. The combination of T2-weighted image-high resolution with mDIXON or diffusion weighted image provided better results for the detection of brachial plexus injuries than mDIXON or diffusion weighted image alone because a combination can detect lesions in both pre- and postganglionic injuries. Limitation of this study, the present study only used the clinical contexts as the reference standard which might be an inaccurate reference. Using a combination of physical examination, surgical findings, and electromyogram as the reference standard might improve the diagnostic yield.Conclusions
MRN with the combination of T2-weighted image-high resolution and mDIXON was superior to conventional myelography for the evaluation of brachial plexus injuries due to its shorter processing times, the lack of a need for contrast medium administration, its noninvasive method, and the provision of information about both preganglionic and postganglionic injuries.Acknowledgements
The study was funded by the Faculty of Medicine Siriraj Hospital.References
1. Balakrishnan G, Kadadi BK. Clinical examination versus routine and paraspinal electromyographic studies in predicting the site of lesion in brachial plexus injury. The Journal of hand surgery. 2004;29(1):140-3.
2. Moran SL, Steinmann SP, Shin AY. Adult brachial plexus injuries: mechanism, patterns of injury, and physical diagnosis. Hand clinics. 2005;21(1):13-24.
3. Carvalho GA, Nikkhah G, Matthies C, Penkert G, Samii M. Diagnosis of root avulsions in traumatic brachial plexus injuries: value of computerized tomography myelography and magnetic resonance imaging. Journal of neurosurgery. 1997;86(1):69-76.
4. Yoshikawa T, Hayashi N, Yamamoto S, Tajiri Y, Yoshioka N, Masumoto T, et al. Brachial plexus injury: clinical manifestations, conventional imaging findings, and the latest imaging techniques. Radiographics : a review publication of the Radiological Society of North America, Inc. 2006;26 Suppl 1:S133-43.
5. Caporrino FA, Moreira L, Moraes VY, Belloti JC, Gomes dos Santos JB, Faloppa F. Brachial plexus injuries: diagnosis performance and reliability of everyday tools. Hand surgery : an international journal devoted to hand and upper limb surgery and related research : journal of the Asia-Pacific Federation of Societies for Surgery of the Hand. 2014;19(1):7-11.
6. Somashekar D, Yang LJ, Ibrahim M, Parmar HA. High-resolution MRI evaluation of neonatal brachial plexus palsy: A promising alternative to traditional CT myelography. AJNR American journal of neuroradiology. 2014;35(6):1209-13.
7. Chhabra A, Thawait GK, Soldatos T,
Thakkar RS, Del Grande F, Chalian M, et al. High-resolution 3T MR neurography
of the brachial plexus and its branches, with emphasis on 3D imaging. AJNR
American journal of neuroradiology. 2013;34(3):486-97.
Figures