1949
Resting-state functional connectivity of hippocampus in patients with drug-resistant idiopathic generalized epilepsy1Department of Radiology, The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China
Synopsis
Previous studies have found altered resting-state functional connectivity in default mode network in drug-resistant patients with idiopathic generalized epilepsy (
Abstract
Introduction: It is estimated that around 15.6-40% of patients with epilepsy have drug-resistant epilepsy (DRE)1. They do not get remission despite standard therapy with antiepileptic drugs (AEDs), resulting in increased risk for premature death, physical injury, psychosocial dysfunction and reduced quality of life. Therefore, exact and early identification of patients with drug-resistant epilepsy would be helpful for clinicians to advocate more effective treatment and counseling to achieve the improved outcome. Neural network disorder has been increasingly recognized and become a key concept of drug-resistant epilepsy. The previous study indicated the presence of reduced default mode network connectivity in idiopathic generalized epilepsy (IGE) and showed that connectivity is further reduced in treatment-resistant epilepsy2. While the mechanism of drug-resistant epilepsy is still not entirely understood. Hippocampus abnormalities are often related to drug-resistant epilepsy. A Recent study showed that the volume of the hippocampus is decreased in IGE patients3. Whether the hippocampus and the related network play an important role in drug-resistant IGE patients need further study.
Methods: Sixty-two patients with IGE-GTCS from Neurology Department of Drum Tower Hospital were included in this study. Seventeen healthy young adults were recruited as normal controls. The resting state functional MRI and structural imaging data were acquired by using 3.0 Tesla MR scanner (Achieva 3.0 T TX dual Medical Systems; Philips Medical Systems, Eindhoven, Netherlands). After over 12-months follow-up, according to the definition of drug-resistant epilepsy by the International League Against Epilepsy4, patients were divided into the following three groups: After standardized and adequate antiepileptic therapy, patients with seizure-free duration three times longer than the longest seizure interictal duration or seizure-free duration over 12 months were identified as drug-sensitive group (DS), otherwise identified as drug-resistant group (DR). And patients with seizure-free duration three times longer than the longest seizure interictal duration and with total seizure-free duration less than 12 months were identified as the uncertain group, which were excluded in this study. The rest-fMRI data were preprocessed by DPARSF, bilateral hippocampus template from AAL were selected as ROIs for calculating functional connectivity (FC). One-way analysis of variance (ANOVA) and Post hoc Tests were performed to detect the differences of FC among the groups. Spearman's Correlation Test and receiver operating characteristic (ROC) were performed to evaluate the correlations between FC and clinical assessments and to determine the discrimination threshold of FC.
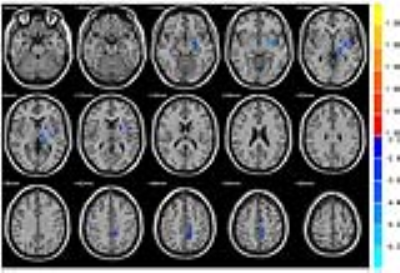
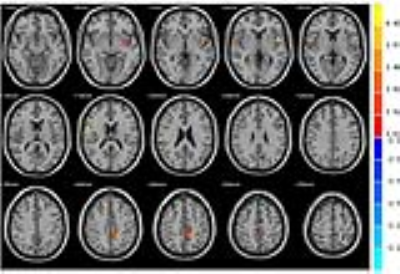
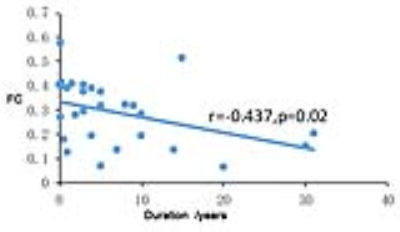
Results: The left thalamus, left putamen, left insular, and right precentral gyrus were found significant difference among the three groups when placing seed in the left hippocampus, while the variable area was found in right precentral gyrus in the right hippocampus. In compared with DS and NC subjects respectively, significant decreased FC was found in DR patients between left hippocampus seed and left thalamus, putamen and left precuneus, while increased FC was found in the DS patients between left hippocampus seed and left putamen, left precuneus and right precentral gyrus in compared with NC patients. In compared with DS, decreased FC were found among DR and NC between right hippocampus seed and right precentral gyrus. The FC between left hippocampus seed and left thalamus-putamen was found to be negatively correlated with duration. ROC curve indicated that the sensitivity to drug-resistant IGE-GTCS of FC between left hippocampus seed and left thalamus-putamen is 100% and the specificity is 89.5%.
Discussion and conclusion: There were much research about hippocampus in temporal lobe epilepsy, and the hippocampus were often related to drug-resistant epilepsy. It is rarely known that Whether the hippocampus and the related network play an important role in drug-resistant IGE patients. Our results showed decreased functional connectivity of bilateral hippocampus in DR IGE patients, and the FC also negatively correlated with seizure duration. It indicated that FC of left hippocampus and left thalamus and putamen were impaired in drug-resistant IGE patients. However, increased FC of the hippocampus was found in DS patients, indicating the functional compensatory of DS patients. The ROC curve suggested that the FC between left hippocampus seed and left thalamus-putamen could be the sensitive and specified indicator of DR patients. The pathological role of the hippocampus in IGE-GTCS, especially in DR patients, could be the irreversible neuronal loss and gliosis within the hippocampus after repeating GTCS result to integrity between the hippocampus and global network and exceeded compensation of the network eventually lead to drug resistance. Therefore, the reduced FC between the hippocampus and global network could be a reliable imaging marker in drug resistance prediction.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant numbers: 81301198, 81401402, 81471643, 81571040, 91649116, 81300925, 81422022, 81271553).References
1. Picot MC, Baldy-Moulinier M, Daurès JP, et al. The prevalence of epilepsy and pharmacoresistant epilepsy in adults: a population-based study in a Western European country. Epilepsia. 2008 Jul;49(7):1230-1238.
2. Kay BP, DiFrancesco MW, Privitera MD, et al. Reduced default mode network connectivity in treatment-resistant idiopathic generalized epilepsy. Epilepsia. 2013; 54(3):461-470.
3. Zhou SY, Tong L, Song F, et al. Selective medial temporal volume reduction in the hippocampus of patients with idiopathic generalized tonic-clonic seizures. Epilepsy Res. 2015;110:39-48.
4. Kwan P, Arzimanoglou A, Berg AT, et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 2010; 51 (6) : 1069-1077.
Figures