1919
Longitudinal assessment of cerebral blood flow change following internal carotid artery revascularization for better prevention of Hyperperfusion syndrome1Radiology and Imaging, Chinese People’s Liberation Army (PLA) General Hospital, Beijing, China, 2General Electric Healthcare, Shang hai, China
Synopsis
Hyperperfusion syndrome (HPS) is a rare but potentially fatal postoperative complication deriving from carotid artery stenting (CAS) and endarterectomy (CEA), while the pattern of post-operation cerebral blood flow (CBF) changes relating to HPS remained unclear. We had used pseudo continuous arterial spin labeling (pCASL) to monitore 4 consecutive time points at 24h, 48h, 72h, and 96h after CEA and CAS in patients with internal carotid artery (ICA) stenosis. We had found that attention should be focused on 72 hours after CAS and 48 hours after CEA to control blood pressure and prevent potential HPS.
Introduction
Carotid artery stenting (CAS) and endarterectomy (CEA) are common treatments for patients with internal carotid artery (ICA) stenosis1,2. Hyperperfusion syndrome (HPS) is a rare but potentially fatal postoperative complication deriving from CEA and CAS3. A number of studies had revealed improvement of cerebral blood flow (CBF) by monitoring one day after CEA and CAS4,5 , while the pattern of post-operation CBF changes relating to HPS remained unclear. In this work, the post-operation CBF was closely monitored at a 24hour interval using pseudo continuous arterial spin labeling (pCASL) in the hope of finding a more suitable scout time point for preventing HPS.Method
From November 2015 to February 2017, thirty-two patients (28 males and 4 females; age=63.0±7.3years) with 50%-99% ipsilateral stenosis in internal carotid artery were enrolled in the retrospective study, out of which 19 patients underwent CAS and 13 patients underwent CEA. Routine MR exams and 3D pCASL (post labeling delay 2.0s) were performed on a 3.0T system within 7 days prior to surgical operations and 4 consecutive time points at 24h, 48h, 72h, and 96h after operations. Blood pressure was kept 110-120/70-80 mmHg for patients during the 24-96h period after operation. A volumetric ICA territory based on gray matter mask according to previous work was extracted to measure mean CBF value of ipsilateral and contralateral side6,7. Linear graphs were used to describe the changes of CBF of ipsilateral and contralateral ICA territory. Comparisons between pre-treatment and 24h-96hours post-treatment CBF values in the treated side with those in the contralateral side separately of CEA and CAS were made using paired t-test. P <0.05 was set considered statistically significant.Results
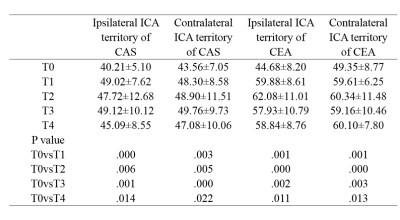
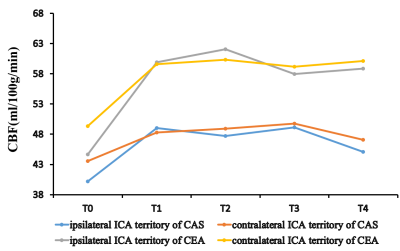
The mean value and standard deviation of pre- and post-operation CBF values in ipsilateral side and contralateral side of CAS and CEA were listed in Table 1. The measured CBF time courses were shown in Figure 1. Among ipsilateral ICA territory of CAS and CEA, contralateral ICA territory of CAS and CEA,the pre-treatment CBF significantly differed from the post-treatment measurements (p < 0.05). All patients presented CBF increment within 24h after operation. At the following time points, CBF values of ipsilateral ICA territory of CAS remained relatively stable on the 48-72 hours then declined on 96 hours; CBF values of ipsilateral ICA territory of CEA maintained an escalating trend during the 48 hours, descended on the 72 hours and remained relatively stable on the 96h; CBF values of contralateral and ipsilateral ICA territory showed similar variation tendencies, but the increase of CBF on contralateral side was smaller than ipsilateral side.Discussion and conclusion
There may be a time period where the HPS is most likely to occur after CEA or CAS, and this knowledge is of great clinical significance for subsequent therapeutic strategies . The values of CBF had a distinguished rise immediately after CEA or CAS, most people showed peak CBF on the ipsilateral side 72 hours after CAS and 48 hours after CEA, which might indicate attention should be focused on the this period to control blood pressure and prevent potential HPS. The synchronized changes of contralateral CBF and the ipsilateral CBF might suggest the formation of primary collateral circulation prior to treatment.Acknowledgements
We thank all the subjects for participating in the study.References
1. Mendelow A D. Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Study Trial (ECST)[J]. Newcastle University, 1998. 2. Bosiers M, Deloose K, Peeters P. Plaque Stability and Carotid Stenting[M]// Practical Carotid Artery Stenting. Springer London, 2009:81-92. 3.Ziaja D, Biolik G, Kocełak P, et al. Neurological symptoms associated with cerebral hyperperfusion syndrome after CEA and CAS--one centre study.[J]. Eur Rev Med Pharmacol Sci, 2014, 18(8):1176-80. 4. Yun T J, Sohn C H, Han M H, et al. Effect of carotid artery stenting on cerebral blood flow: evaluation of hemodynamic changes using arterial spin labeling[J]. Neuroradiology, 2013, 55(3):271-281. 5. Ances B M, Mcgarvey M L, Abrahams J M, et al. Continuous arterial spin labeled perfusion magnetic resonance imaging in patients before and after carotid endarterectomy.[J]. Journal of Neuroimaging, 2004, 14(2):133. 6.Nowinski W L, Qian G, Kirgaval Nagaraja B P, et al. Analysis of Ischemic Stroke MR Images by Means of Brain Atlases of Anatomy and Blood Supply Territories[J]. Academic Radiology, 2006, 13(8):1025-34. 7. Lee J S, Lee D S, Kim Y K, et al. Probabilistic map of blood flow distribution in the brain from the internal carotid artery.[J]. Neuroimage, 2004, 23(4):1422-1431.
Figures