1916
Cerebral blood flow in different severity degree moyamoya disease before and after artery bypass surgery1Liaocheng People’s Hospital, Liaocheng, China, 2GE Healthcare, MR Research China, Beijing, China
Synopsis
The goal of the present study was to assess the improvement of CBF after STA-MCA bypass surgery in the mid, moderate, and severe regions based on Tmax value in Moyamoya disease patients. For this purpose, 13 Moyamoya patients were scanned using 3D pc-ASL, and the different perfusion territories were separated based on ASPECT scoring system. The results indicate that mid regions did not get obvious CBF improvement after the surgery and the mid patients did not need to get the bypass surgery.
Introduction
Surgical revascularization is a common treatment method for patients with moyamoya disease (MMD) and direct bypass, mostly connecting superficial temporal artery (STA) to middle cerebral artery (MCA), is useful for improving cerebral blood flow.1Ischemia symptom is conventionally used as surgery indication, but it’s not applicable for patients suffering artery stenosis presenting mild or no symptoms. Time to maximum (T-max) delay has been used to assess the severity of ischemia condition with prolonged delay time indicating severe ischemia condition.1, 2This work aims to use arterial spin labeling (ASL) technique to assess the hemodynamic change after STA-MCA bypassing surgery and study its relation with T-max delay time.Methods
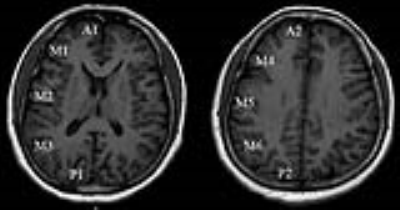
Thirteen patients diagnosed with MMD underwent STA-MCA bypass surgery were recruited for this study. All the patients were absence of major cerebral infarction, as confirmed in T2-FLAIR. Routine MR exams and ASL were performed for these patients before and after bypass surgery in 7 days to 14 days with a 3.0T whole body system (MR 750W, GE). The ASL parameters were listed as follows: labeling duration 1450ms, and post labeling delay 2025ms, 3D stack of spiral fast spin echo acquisition with 8 arms, 512 points per arm, and 3 NEX. Regional CBF of cortical tissue were extracted from 10 perfusion territories based on ASPECTS segmentation (Albert Stroke Program Early Computed Tomography Score, 2 anterior, 6 middle, and 2 posterior), as demonstrated in Figure.1. The severity of each region was graded into three groups based on T-max value acquired from computed tomography perfusion (CT Revolution, GE): mild delay with T-max between 3 to 5 second; moderate delay with T-max between 5 to 8 second; and severe delay with T-max exceeding 8 second. CBF from 130 regions were measured from 13 patients.Results
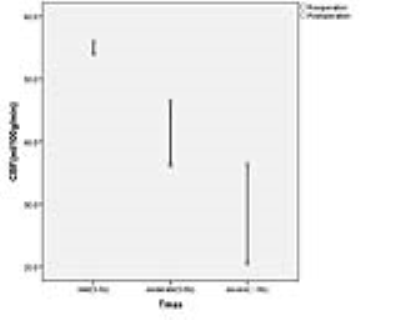
The normal, mild, moderate, and severe delay regions were about 2% (2/130), 35% (46/130), 40% (52/130), and 23% (30/130). All regions had an increase of CBF value after the surgery except M1,M4,P1andP2 region(M1,p=0.361; M4,p=0.229; P1,p=0.375; P2,p=0.095;) A significant CBF improvement was observed in severity group (+15.96±15.75) compared to moderate group (+9.45±13.88, p<0.01) and mild group(+1.77±12.85, p<0.01), as shown in Figure.2. Among the regions defined in ASPECTS, M2, M5 and A2 features the highest CBF increment, as shown in Figure.3.Discussion and Conclusion
Direct bypass surgery is useful to improve hemodynamics, and the collateral blood folw was redistributed after surgery, 3 and ASL can show the variation of CBF and presence of the collateral perfusion.4 In mild regions of this study, the effectivity of the operation was not remarkable, but in severe regions and morderate regions, the bypass artery (in another form, it was artificial collateral artery) given great help to fed the cortex. The mild patients have extensive collateral perfusion,1 operation was not necessary to improve blood supply. ACA territory may accept blood from MCA territory through the pial anastomosis, such as A2 territory benefit from the STA-MCA bypass in this study.3 The limitation of this study is single-PLD ASL has limitation of underestimating CBF in cortical region, and the short outcome of CBF change is not obvious in some patients, so long outcome of CBF must be followed up in this study.Acknowledgements
No acknowledgement found.References
1. Fan AP, Guo J, Khalighi MM, et al. Long-Delay Arterial Spin Labeling Provides More Accurate Cerebral Blood Flow Measurements in Moyamoya Patients: A Simultaneous Positron Emission Tomography/MRI Study. Stroke. 2017;48(9):2441-2449.
2. Olivot JM, Mlynash M, Zaharchuk G, et al. Perfusion MRI (Tmax and MTT) correlation with xenon CT cerebral blood flow in stroke patients. Neurology. 2009;72(13):1140-5.
3. Kuroda S, Houkin K. Bypass surgery for moyamoya disease: concept and essence of sugical techniques. Neurologia medico-chirurgica. 2012;52(5):287-94.
4. Zaharchuk G, Do HM, Marks MP, Rosenberg J, Moseley ME, Steinberg GK. Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with moyamoya disease. Stroke. 2011;42(9):2485-91.
Figures