1909
The usefulness of thick slice-basal ganglia rapid pCASL for acute ischemic stroke.1Department of Radiology, Otaru General Hospital, Otaru, Japan, 2Department of Neurosurgery, Otaru General Hospital, Otaru, Japan, 3Department of Neurosurgery, Hokkaido University Graduate School of Medicine, Sapporo, Japan
Synopsis
In this study, we demonstrated the efficacy of the thick slice-basal ganglia pCASL (TB-pCASL) for acute ischemic stroke. The limited scan range and selection of thick slice retain signal noise to ratio (SNR) even in approximately 1min scan. TB-pCASL can rapidly estimate an ischemic region corresponding occlusion-stenosis region, and to combine with DWI can depict penumbra within 2min. TB-pCASL is reliable and useful tool for diagnosis of acute ischemic stroke in the emergency medical field.
Introduction
The efficacy of endvascular therapy for acute ischemic stroke (AIS) caused by large vessel occlusion.1,2 Time to re-perfusion is crucial to obtain a good outcome. 3 The penumbra which is identified as DWI-Perfusion mismatch4 has been the most important factor to decide whether or not to apply the endovascular treatment. Pseudo continuous Arterial spin labeling (pCASL) is wide spreading as a non invasive perfusion method with MRI. However, the standard sequence of the whole-brain pCASL needs 5 min in general. 5,6 Therefore, short time pCALS is desired in the emergency medical field. The purpose of this study is to construct the rapid pCASL, and to confirm its accuracy of visualization of ischemic region.Method
[MRI] Ingenia 3.0T (PHILIPS, Best, the Netherland).
[Image Analysis software] ImageJ (National Institutes of Health, Bethesda, Maryland, USA)
[Statical analysis software] JMP version 12 (SAS Institute Inc., Cary, NC, USA.)
[Thick slice-Basal-ganglia pCASL (TB-pCASL)]
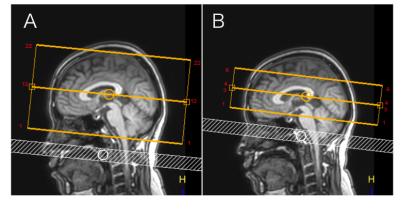
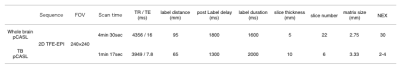
We attempted to reduce scan time of pCASL by limited scan range and thick slice selection. The outlines of TB-pCASL comparing with whole-brain pCASL was shown in Figure 1. We selected 10mm slice thickness, and scan rage was limited on the basal-ganglia. Other parameters were shown in Figure 2.
1) Healthy volunteers study
TB-pCASL and whole-brain pCASL were performed in 5 volunteers (3 men and 2 women; mean age, 36 years; range, 26–50 years). TB-pCASL was achieved by changing the NSA from 2 to 14. The SNR of the brain tissue was measured at the basal-ganglia slice using ImageJ by two radiological technicians. We further explored the scan setting that could retain the equivalent SNR compared with whole-brain pCASL. Finally, the setting that had a sufficient SNR and a shorter scanning time was selected as the optimized protocol. The whole-brain pCASL used the standard settings recommended by the manufacturer. Dunnett’s test was performed to compare SNR of TB-pCASL by the changing of NSA. (p < 0.005)
2) Clinical patients study
MRI routine protocol including optimized TB-pCASL was performed in patients suspected with AIS. Firstly, two radiological technicians estimated the image quality using a 5-point scale method. The criteria was shown in Figure 3. Secondly, Two neurosurgeons defined an occlusion-stenosis site estimated from the ischemic region on TB-pCASL. We evaluated the correlation between an ischemic region of TB-pCASL and an occlusion or stenosis site diagnosed on DSA. Weighted κ test with calculation of 95% confidence interval was used to evaluate the inter-observer agreement between an ischemic region of TB-pCASL and an occlusion-stenosis site on DSA. (p < 0.005)
We performed the studies of healthy volunteers and clinical patients under a protocol approved by the Institutional Review Board of Otaru General Hospital.
Result
1) Healthy volunteer study
The SNR of TB-pCASL was the equivalent on NSA 6–14. We selected NSA = 10 as the optimized setting, considering that the scan time and patient will be older than that of volunteers in general. The scan time was 1 min and 17 sec.
2) Clinical patient study
30 patients participated in our study. (12 men and 18 women; mean age was 80.5 ± 8.53 years). In all patients, TB-pCALS was performed successfully.
2-1) Image quality
The average score using a 5-point scale method corresponded to 3.75. There was a good agreement between the two technicians.
2-2) The estimation of an ischemic region on TB-pCASL
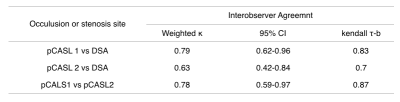
The summarize of result was shown in Figure 4.
There was overall a strong agreement among reader 1, reader 2, and DSA. The κ coefficient and 95% confidence interval (CI) were as follows: between reader 1 and DSA, κ = 0.79; between reader 2 and DSA, κ = 0.63; and between reader 1 and reader 2, κ = 0.78. The ischemic region could be estimated in all cases using the basal-ganglia pCASL.
Discussion
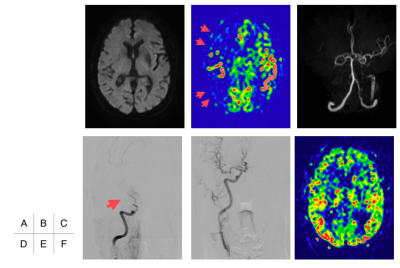
SNR was retained even in shorter scan time such as approximately 1min. Slice-thickness was selected 10mm, moreover, shorter post label distance decreased T1 recovery of the labeled blood exponentially. Scan range was not much different comparing general CT-perfusion. An ischemic region corresponding occlusion-stenosis site was depicted correctly even in 1min scan. The typical case who demonstrated the efficacy of TB-pCASL is shown in Figure 5. An ischemic region corresponding right middle cerebral artery can be confirm in only TB-pCASL.Conclusion
We constructed a rapid pCASL protocol covering only the basal ganglia. This sequence could be acquired within approximately min, demonstrate an ischemic region in correct. Therefore, this study indicate that thick slice-basal ganglia rapid pCASL is a reliable sequence for acute ischemic stroke.Acknowledgements
No acknowledgement foundReferences
1. Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009-1018.
2. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019-1030.
3. Sheth SA, Jahan R, Gralla J, et al. Time to endovascular reperfusion and degree of disability in acute stroke. Ann Neurol 2015; 78: 584-593.
4. Schaefer PW, Barak ER, Kamalian S, et al. Quantitative assessment of core/penumbra mismatch in acute stroke: CT and MR perfusion imaging are strongly correlated when sufficient brain volume is imaged. Stroke 2008; 39: 2986-2992.
5. Deibler AR, Pollock JM, Kraft RA, et al. Arterial spin-labeling in routine clinical practice, part 1: technique and artifacts. AJNR Am J Neuroradiol 2008; 29: 1228-1234.
6. Zaharchuk G. Arterial spin-labeled perfusion imaging in acute ischemic stroke. Stroke 2014; 45: 1202-1207.
Figures

The criteria of image quality.
Excellent (5-point): the sufficient signal noise to ratio (SNR) which can be distinguished between white matter and gray matter was retained. In addition, the motion artifact was not observed.
Good (3-point): SNR which can be observed a brain tissue was retain although white matter and gray matter could not be distinguished. In addition, a few motion artifact was included.
Poor (1-point): SNR was poorly, or there was a significant motion artifact. Therefore, brain tissue could not be observed at all.