1901
Visualizing Wall Enhancement Over Time in Unruptured Intracranial Aneurysms Using 3D Vessel Wall Imaging1UCSF, San Francisco, CA, United States
Synopsis
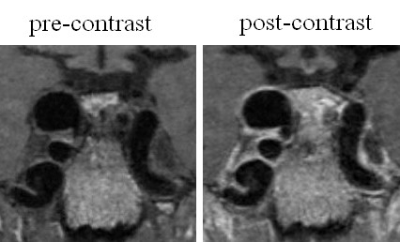
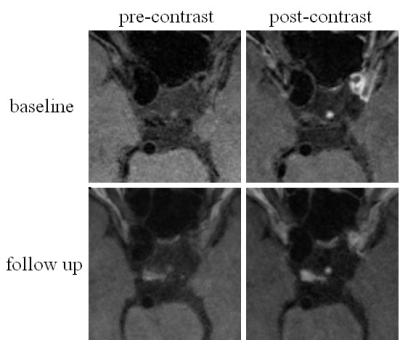
Advances in vessel wall imaging techniques using high-resolution MR sequences now allow for improved visualization of the walls of intracranial vessels. In this study, we present results obtained with a 3D SPACE to visualize the walls of intracranial aneurysms and to grade the extent of aneurysm wall enhancement in subjects whose aneurysms were monitored over time. Our studies showed that visualization of the aneurysm wall is significantly better on post-contrast images than on pre-contrast images, and the majority of unruptured aneurysms show wall enhancement. Furthermore, we found the wall enhancement scores to remain essentially unchanged on follow up studies.
Purpose
High resolution MRI vessel wall imaging provides important capabilities in assessment of intracranial vascular disease including intracranial aneurysms. This study aims to compare the aneurysm wall visualization on pre- and post- 3D isotropic T1-weighted fast-spin-echo sequence (SPACE) images and to explore whether there is a change in wall enhancement at follow up.Methods
Twenty-nine patients with thirty-five unruptured intracranial aneurysms were scanned on a 3T Siemens Skyra scanner with pre- and post-contrast 3D T1-weighted SPACE (0.5mm isotropic). Follow up studies were performed on all patients. Aneurysm wall visibility and enhancement scores were assigned by three neuroradiologists on pre- and post-contrast SPACE respectively. The aneurysm wall visibility between pre- and post-contrast images as well as the wall enhancement between follow up and baseline studies were compared. Differences in wall visibility and enhancement were also investigated as a function of aneurysm diameter and location.Results
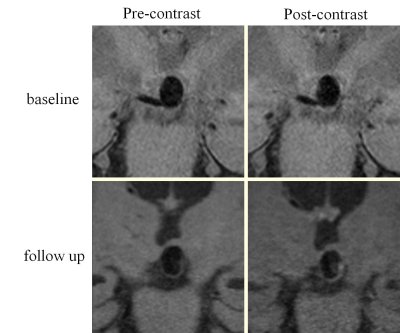
Agreement among three reviewers in grading wall visibility and enhancement was excellent. Post-contrast images had significantly higher wall visibility compared to pre-contrast images. A wall enhancement score ≥2 was found on 71% (25/35) of the aneurysms. Changes in levels of wall enhancement were found on 17% (6/35) of the aneurysms at follow up studies, but those changes were small. The wall of large aneurysms (≥7mm) was better visualized than small aneurysms. Wall enhancement scores of large aneurysms were significantly higher than that of small aneurysms. There was no significant differences in aneurysm wall visibility and enhancement between different locations. Enhancement patterns were relatively stable over time.Discussion
It is expected that improved characterization of the aneurysm wall will provide insights into the likelihood that a specific aneurysm might grow over time, and importantly whether an aneurysm is at increased risk for rupture. The studies were acquired with isotropic high spatial resolution (0.5mm) of 3D SPACE. An understanding of intracranial vessel wall response to the administration of gadolinium-based contrast agents is incomplete. There is a consensus opinion that this enhancement is likely related to inflammatory status[1]. Yet the response is non-specific, and, in particular, vessels that are apparently otherwise healthy can also show some degree of enhancement. Nevertheless, there are reports that aneurysm wall enhancement might be strongly correlated with rupture[2]. In this study, wall enhancement (score≥2) was detected on 70% of the 35 unruptured aneurysms. This result differs from previous reported studies. However, the wall enhancement was on average found to cover less than 50% of the aneurysm wall area (average score: 2.34±1.16). As these aneurysms were stable (no growth over time), further studies are needed to identify the difference in wall enhancement degree between stable and unstable aneurysms. Our results indicated that the walls of large aneurysms are better visualized than those of small ones. We also find that there was greater wall enhancement in larger aneurysms. The reason for improved vessel wall visibility in larger aneurysms may be that the aneurysm wall thickness might increase as the aneurysm diameter increases[3]. We also divided patients into three groups based on aneurysm location. Differences in visibility and enhancement of the aneurysm wall did not reach statistical significance by location. However, this could be related to the small number of aneurysms in each group. Besides, this might also reflect the heterogeneity in wall thickness in these different locations. Follow-up imaging should be considered in patients with conservatively managed unruptured aneurysms to evaluate aneurysm growth[4]. In our study, 4 of the 6 aneurysms that had different enhancement scores at follow up showed changes of only one grade. Two showed changes of up to 2 grades, and of these one increased in enhancement over time while the other decreased. Furthermore, only 1 of the 6 aneurysms that showed any enhancement change were ≥7mm. Due to the small number of aneurysms demonstrating any change in contrast enhancement, it remains unclear the extent to which enhancement patterns are stable over time in asymptomatic, stable aneurysms; however, our study suggests that if there are any changes they are relatively small.Conclusion
3D T1-weighted high resolution SPACE can be used to evaluate vessel wall characteristics in intracranial aneurysms patients and assess changes in enhancement at follow up studies. Imaging with SPACE following contrast administration provides better aneurysm wall visibility and improves diagnostic confidence.Acknowledgements
we have nothing to disclouse.References
[1] Hu P, Yang Q, Wang DD, Guan SC, Zhang HQ. Wall enhancement on high-resolution magnetic resonance imaging may predict an unsteady state of an intracranial saccular aneurysm. Neuroradiology. 2016;58:979-985. [2] Nagahata S, NagahataM, ObaraM, et al. Wall enhancement ofthe intracranial aneurysms revealed by magnetic resonance vesselwall imaging using three-dimensional turbo spin-echo sequencewith motion-sensitized driven-equilibrium: a sign of ruptured aneurysm? Clin Neuroradiol. 2016; 26(3): 277-283.
[3] Song J, Park JE, Kim HR, Shin YS. Observation of cerebral aneurysm wall thickness using intraoperative microscopy: clinical and morphological analysis of translucent aneurysm. Neurol Sci. 2015;36:907-912. doi: 10.1007/s10072-015-2101-9.
[4] Etminan N, Brown RD Jr, Beseoglu K, Juvela S, Raymond J, Morita A, et al. The unruptured intracranial aneurysm treatment score: a multidisciplinary consensus. Neurology. 2015;85:881-889. doi: 10.1212/WNL.0000000000001891.
Figures