Michael L Rohan1, Clara Wellons2, Megan Shevenell3, Nicolette Schwarz4, Xingfeng Shao5, Daniel JJ Wang5, and Blaise Frederick3
1Imaging, McLean Hospital, Belmont, MA, United States, 2imaging, McLean Hospital, Belmont, MA, United States, 3McLean Hospital, Belmont, MA, United States, 4Mc:ean Hospital, Belmont, MA, United States, 5University of Southern California, Los Angeles, CA, United States
Synopsis
Arterial Spin Labeling (ASL) measurements are
employed here in a suite of hemodynamic assessments in our study of cerebrovascular
reactivity. In this project we test a 3D Gradient and Spin Echo (GRASE)
Multiple delay Pseudo-Continuous Arterial Spin Labeling (MPCASL) Magnetic
Resonance (MR) acquisition in order to measure the change in these measures
under gas challenge. Subjects were scanned with 3D GRASE MPCASL while breathing
medical air, oxygen, or Carbogen (5% CO2 +95% O2) under controlled conditions. Changes
in blood flow, volume, and arrival time that were observed will be used to
calibrate novel delay assessment methods.
Introduction
Brain health requires that the cerebral vasculature be able
to supply an appropriate amount of oxygen and nutrients to brain tissue under a
wide range of physiological conditions. These conditions include both the normal
resting baseline state, and states with higher oxygen requirements, such as
high cognitive load; to meet this requirement, the vasculature undergoes
autoregulatory vasodilation to respond to increase demand. Cerebrovascular
reactivity (CVR) is the brain blood vessels’ capacity for vasodilation. It
offers useful clinical information in patients at risk for cerebral ischemia
associated with chronic stenosis or occlusion of cerebral blood vessels,
patients at risk of ischemia in deep white matter, which leads to sub-cortical
infarction, and may reflect abnormalities in diabetes, and in patients with
dementing illnesses including Alzheimer’s disease. Assessment of hemodynamic
impairment may be critical to informing management decisions in patients with
atherosclerotic disease, and neuroimaging is performed routinely in the
evaluation of these patients. This project will calibrate our MPCASL sequence
and methodology using Oxygen and Carbon dioxide gas challenges to simulate
vascular pathology.
Arterial Spin Labeling is an MRI technique used to study
cerebral blood flow and hemodynamics. In this project we use static ASL to
assess hemodynamic parameters such as cerebral blood flow (CBF), cerebral blood
volume (CBV), and bolus arrival time. In order to simulate pathology we perform
these measures in healthy controls while breathing medical air (MA), Oxygen (100%
O2), or Carbogen (5% CO2 / 95% O2). Oxygen is a vasoconstrictor and carbon
dioxide is a vasodilator; and we expected both increases and decreases in
hemodynamic parameters to occur under these gas challenges. We expect O2 to
have minimal effects on CBF and CBV; we expect Carbogen to cause increases in
CBF and in bolus arrival time.Methods
We collected multi-delay PCASL data using a 3D Gradient and
Spin Echo (GRASE) sequence on a Siemens 3T Prisma MR system. 3D GRASE provides
higher resolution within achievable scan times. The acquisition used 8 single
volume delays with TE=30ms, TR=4s, TI = 1.6s, 2.0s, 2.4s, 2.8s, 3.2s, 3.6s,
4.0s and 4.4s; the tag duration was 1.5s (within TI); isotropic voxels were
3.5mm with a matrix of 64x64x40; scan time was 5:30. Three acquisitions were
made. Subjects were breathing either MA, O2 or Carbogen through an MR
compatible portable tank-based apparatus utilizing a demand regulator during
each scan. The sequence provided both tag and control images as well as M0
images. A standard 3D anatomic image was also acquired for registration. Data
were acquired from five healthy subjects.
Calibrated ASL processing was performed using FSL BASIL
software (OSFORD FMRIB v5.0.10) which provided maps of voxel wise bolus arrival
time, quantitative CBF and quantitative CBV. Assessments were made of the three
hemodynamic parameters in a gray matter (GM) region and in a region containing
the basal ganglia and thalamus (BG). These two regions were selected because
they represent different tissue vasculature and variability for comparison.
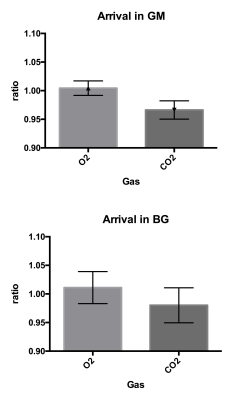
Regional mean values were compared for CBF and CBV, while voxel wise maps of
the relative change in arrival time from MA to O2 and MA to Carbogen were made
to assess change in arrival time.Results
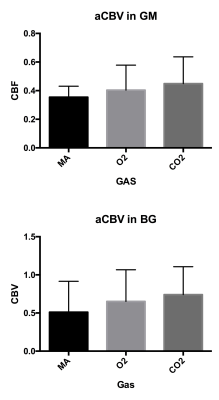
Changes in CBF were apparent with a reduction in regional
CBF observed under O2 as compared to MA, 18.5% in both GM and the BG; there was
an increase in CBF under Carbogen in GM (16.5%) and in the BG (6%). CBV
increased under the influence of both gases, with a 13.8% increase under O2 in
GM and a 27.8% increase under O2 in the BG, and an increase by 26.8% under
Carbogen in the GM and by 45% in the BG. Arrival times were unchanged in both
regions under O2 and were decreased by 3% in the GM and by 2% in the BG under
Carbogen. The regional mean changes are shown in the figures below (CBF and
CBV) as well as the mean voxel wise change in bolus arrival times.Discussion
The repeatability and robustness of these results
demonstrate that the 3D GRASE sequence can be used to detect the desired changes
in cerebrovascular reactivity. Reduction in CBF under the influence of O2
occurred as expected, and the increase in CBF under the influence of the carbon
dioxide in the Carbogen mix was also as expected. The increase in CBV under
both gases was not expected and further modeling will be performed to explain
this. The changes in bolus arrival time were small but robust.Acknowledgements
No acknowledgement found.References
Donahue,
M.J., et al., Bolus arrival time and cerebral blood flow responses to
hypercarbia. Journal of
cerebral
blood flow and metabolism : official journal of the International Society of
Cerebral Blood Flow
and
Metabolism, 2014. 34(7): p. 1243-1252.
Alsop,
D.C., et al., Recommended implementation of arterial spin-labeled perfusion MRI
for clinical
applications:
A consensus of the ISMRM perfusion study group and the European consortium for
ASL
in
dementia. Magnetic resonance in medicine : official journal of the Society of
Magnetic Resonance in
Medicine
/ Society of Magnetic Resonance in Medicine, 2014.
Wang et al. Neuroimage Clin. 2013;3:1-7