1813
Resting-state brain functional alteration in dorsal attention network associated with post-chemotherapy breast cancer1Institute of Medicine, Chung Shan Medical University, Taichung, Taiwan, 2Department of Medical Imaging and Radiological Sciences, Chung Shan Medical University, Taichung, Taiwan, 3Department of Medical Imaging, Chung Shan Medical University Hospital, Taichung, Taiwan, 4School of Medicine, Chang Gung University, Taoyuan, Taiwan, 5Department of Psychiatry/ Health Information and Epidemiology Laboratory, Chang Gung Memorial Hospital, Chiayi, Taiwan, 6Breast Center, Taichung Tzu Chi Hospital, Taichung, Taiwan, 7Division of Thoracic Surgery, Department of Surgery, Chung Shan Medical University Hospital, Taichung, Taiwan, 8Department of Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan
Synopsis
The current study was to investigate post-chemotherapy breast cancer with rs-fMRI using mfALFF analysis and correlated with clinical cognitive testing. The results showed altered brain activity in the dorsal attention network in breast cancer patients compared to healthy controls and the affected areas were associated with MMSE, CAMS-R and IES-R scores.
Introduction
Currently, breast cancer is the most common cancer among women all over the world. Adjuvant chemotherapy has significantly reduced mortality but increased cognitive impairments, resulting in important considerations of the quality of life issues 1-4. The aim of this study was to investigate breast cancer patients (BCs) undergoing chemotherapy treatment with resting-state functional MRI (rs-fMRI) using mean fractional amplitude of low-frequency fluctuations (mfALFF) analysis 5, and correlated with clinical cognitive testing to explore the conceivable underlying mechanism of the cognition alternations.Methods
Nineteen pathological diagnosed breast cancer women (BCs) treated with standard chemotherapy (Taxotere and Epirubicin) within 6 months and 20 age-matched female healthy controls (HCs) were recruited in this study. The study was approved by the Institutional Review Board of Chung Shan Medical University Hospital and Taichung Veterans General Hospital. All subjects participated in the study after providing informed consent.
All the participants underwent rs-fMRI scan (GRE-EPI, TR/TE = 2000ms / 30ms, voxel size= 3.4×3.4×4.0 mm3, 33 axial slices per volume, total 256 volumes per scan) using 1.5 T MRI scanner (Magnetom Aera, Siemens Medical Systems, Germany) with a standard 8-channel head coil.
After functional image pre-processing process, mfALFF (frequency range from 0.01 to 0.12 Hz) was used for further data analysis with Statistical Parametric Mapping 8 (SPM8, Wellcome Department of Cognitive Neurology, London, UK). Two-sample t-test was used to assess the difference in mfALFF between the BCs and HCs and multiple regression was used to investigate the relationship between the mfALFF and the clinical cognitive testing, including Mini-Mental State Examination (MMSE), Cognitive and Affective Mindfulness Scale-Revised (CAMS-R) and Impact of Event Scale-Revised (IES-R). A p-value less than 0.05 was considered statistically significant.
Results
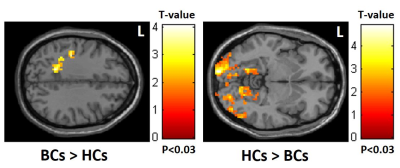
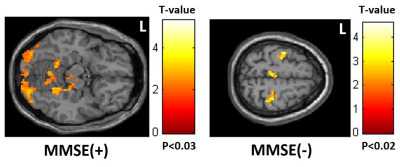
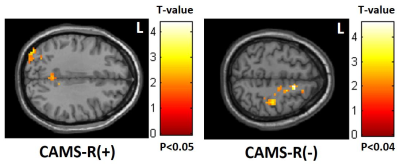
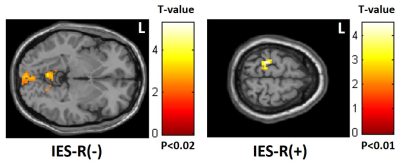
Altered brain activity in the dorsal attention network (DAN) was found, which showed decreased mfALFF over occipital lobe, including primary visual cortex, but increased mfALFF over frontoparietal lobe, including prefrontal cortex (PFC) and posterior parietal cortex (PPC) in BCs compared to HCs (Fig. 1). In clinical cognitive testing correlation analysis, positive correlation between MMSE/ CAMS-R scores and mfALFF in occipital lobe but negative correlation in frontoparietal lobe (Fig. 2, 3). In contrast, positive correlation between IES-R scores and mfALFF in frontoparietal lobe but negative correlation in occipital lobe were found (Fig. 4).Discussion
In this cross-section study based on rs-fMRI, mfALFF alterations 6-months post-chemotherapy BCs were observed in the DAN compared to HCs and were correlated to clinical cognitive testing. Changes in connectivity in the DAN have implications for understanding the impact of chemotherapy on cognitive performance, the DAN is involved in the top-down, voluntary control of attention. Regions in this network have been shown to be involved in working memory and attention using both task-based fMRI and arterial spin labeling perfusion MRI in early post-chemotherapy BCs 6,7. The concept of top-down orientating of DAN drives from the Rolandic area and reacts at the occipital lobe may help to explain our results that during rs-fMRI study, the requirement of asking participants to think of nothing, may drive the DAN to achieve the goal and the BCs group may tend to use more effort but get less response compared to the HCs, which result in increased mfALFF in the Rolandic area and decreased mfALFF in the occipital lobe. In contrast, we did not find significant difference in ventral attention network (VAN) between the two groups. Previous studies in type 2 diabetes mellitus and Alzheimer's disease also showed similar results that fewer significant correlations between VAN and cognitive performance 8,9. Therefore, we suggested that VAN is relatively stable and less susceptible to the impact of BCs post-chemotherapy compared with DAN. The results of clinical cognitive testing correlation analysis indicated that DAN plays an important role in both cognitive function and attention alterations.Conclusion
Our results suggested that altered mfALFF in the DAN in midterm post-chemotherapy BCs and potentially related to clinical cognitive assessments.Acknowledgements
This study was supported by the research programs MOST106-2221-E-182-079, MOST104-2314-B-040-001 and NSC103-2420-H-040-002, which were sponsored by the Ministry of Science and Technology, Taipei, Taiwan. This work was also supported by the research programs NMRPD1G1321 and CORPG6G0101, which were sponsored by Chang Gung University, Taoyuan, Taiwan and Chang Gung Medical Foundation, Chang Gung Memorial Hospital, Chiayi, Taiwan.References
1. Reuter-Lorenz PA, Cimprich B. Cognitive function and breast cancer: promise and potential insights from functional brain imaging. Breast Cancer Res Treat. 2013;137(1):33-43.
2. Cheung YT, Tan EH, Chan A. An evaluation on the neuropsychological tests used in the assessment of postchemotherapy cognitive changes in breast cancer survivors. Support Care Cancer. 2012;20(7):1361-1375.
3. Wefel JS, Vardy J, Ahles T, et al. International Cognition and Cancer Task Force recommendations to harmonise studies of cognitive function in patients with cancer. Lancet Oncol. 2011;12(7):703-708.
4. Wefel JS, Lenzi R, Theriault RL, et al. The cognitive sequelae of standard-dose adjuvant chemotherapy in women with breast carcinoma: results of a prospective, randomized, longitudinal trial. Cancer. 2004;1;100(11):2292-2299.
5. Zou QH, Zhu CZ, Yang Y, et al. An improved approach to detection of amplitude of low-frequency fluctuation (ALFF) for resting-state fMRI: fractional ALFF. J Neurosci Methods. 2008;15;172(1):137-141.
6. Chen X, He X, Tao L, et al. The attention network changes in breast cancer patients receiving neoadjuvant chemotherapy: Evidence from an arterial spin labeling perfusion study. Sci Rep. 2017;17;7:42684.
7. Dumas JA, Makarewicz J, Schaubhut GJ, et al. Chemotherapy altered brain functional connectivity in women with breast cancer: a pilot study. Brain Imaging Behav. 2013;7(4):524-532.
8. Xia W, Wang S, Rao H, et al. Disrupted resting-state attentional networks in T2DM patients. Sci Rep. 2015;8;5:11148.
9. Li R, Wu X, Fleisher AS. et al. Attention‐related networks in Alzheimer’s disease: A resting functional MRI study. Hum Brain Mapp. 2012;33(5):1076-1088.
Figures