1809
Assessment of brain volume and shape abnormalities in the major depressive disorders with and without suicidal ideation1Department of Medical Imaging and Radiological Sciences, Chung Shan Medical University, Taichung, Taiwan, 2School of Medicine, Chang Gung University, Taoyuan, Taiwan, 3Department of Psychiatry/ Health Information and Epidemiology Laboratory, Chang Gung Memorial Hospital, Chiayi, Taiwan, 4Department of Diagnostic Radiology, Chang Gung Memorial Hospital, Chiayi, Taiwan, 5Department of Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan
Synopsis
There is very strong connection between patients with major depressive disorders (MDD) and suicide. We used voxel-based morphometry (VBM) and vertex-wise shape analyses to observe the difference between the MDD patients with and without suicidal ideation in their brain volume of gray and white matter as well as shape. We found the negative correlation between the brain volume of limbic system in MDD patients. We also found the significant difference in brain volume and shape of limbic system between suicidal ideation and non-suicidal ideation.
Introduction
Patients with major depressive disorders (MDD) have a high risk of completed or attempted suicide. Multiple neuroimaging methods have been employed to investigate the neural circuitry of suicide-related thoughts and behaviors. Previous study used diffusion tensor imaging (DTI) to investigate the structural integrity of WM connections 1. Several functional neuroimaging methods, such as functional magnetic resonance imaging (fMRI), have been used to study regional brain activity, functional connectivity, and neurotransmitter function 2. However, the understanding of the MDD patients with and without suicide ideation remains far from complete. Therefore, we tried to find the brain volume and shape changes between suicidal ideation and non-suicidal ideation patients using voxel-based morphometry (VBM) and vertex-wise shape analyses.Methods
We examined 56 MDD patients’ brain with MRI, including 27 suicidal ideation and 29 non-suicidal ideation, and 56 matched healthy controls. MRI examinations were performed on 112 people with a 3T imaging system (Verio, Siemens, Germany). Hamilton Depression Rating Scale (HAM-D) and Hospital Anxiety and Depression Scale (HADS) were examined. The Magnetization Prepared Rapid Gradient Echo Imaging (MPRAGE) sequence was used to obtain the T1-weighted image with following parameters: TR = 3500 ms, TE = 2.87 ms, TI = 1100 ms, voxel size (resolution) = 0.9 x 0.9 x 0.9 mm3, and scan time = 7.11 min.
In VBM analysis, all structural data were processed using Statistical Parametric Mapping 8 (SPM8, Wellcome Department of Cognitive Neurology, London, UK) with Voxel-Based Morphometry 8 (VBM8, University of Jena, Department of Psychiatry, Jena, Germany) toolbox. Each raw data was first normalized to International Consortium for Brain Mapping (ICBM) templates, East Asian Brain. Whole-brain T1-weighted images were then segmented into gray matter and white matter. The multiple regression was performed the obtain the correlation between brain volume of gray/white matter and HAM-D/HADS in all participants. To avoid the original difference of each brain, sex and whole brain volume were used as covariates. Then, we divided 56 MDD patients into 27 suicidal ideation and 29 non-suicidal ideation, and also recruited 56 matched healthy controls. The t-test was used to indicate the difference of gray and white matter volume between each group.
In the vertex-wise shape analysis, FMRIB Software Library (FSL, Oxford, UK) was performed to subcortical segment the brain into 15 specific structures based on T1-weighted MRI scans using shape and appearance models. Then vertex-wise analysis was used to show the location of differences in the shape of subcortical structures between each group.
Results
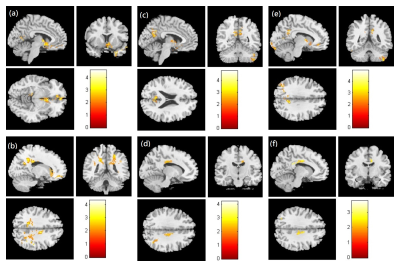
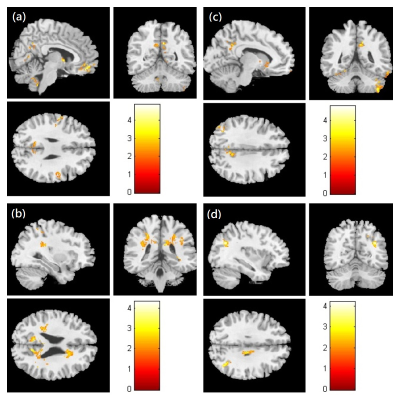
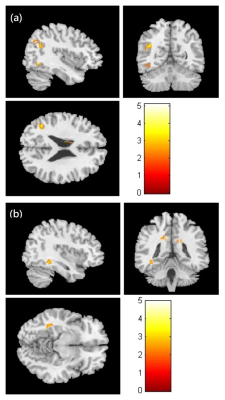
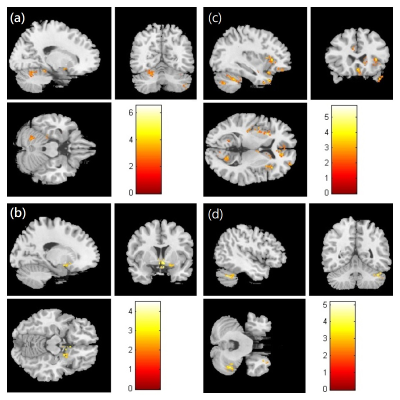
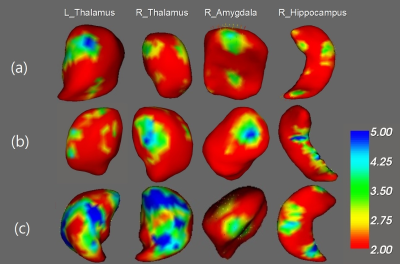
We observed the negative correlation between HAM-D/HADS scales and brain volume of gray/white matter in the limbic lobe (Fig. 1). A negative correlation between HAM-D/anxiety scales and brain volume of gray/white matter was also found in the parietal lobe (Fig. 2). We also found the volume of both gray and white matter in temporal lobe was smaller in the suicidal ideation patients compared with non-suicidal ideation (Fig. 3). The volume of gray matter in frontal lobe and cerebellum was smaller in both suicidal ideation and non-suicidal ideation patients compared with healthy controls (Fig. 4). In the shape analysis, the significant difference of bilateral thalamus, right amygdala and right hippocampus was found between each group (Fig. 5). Above results were all statistically significant (corrected p < 0.05).Discussion
We found that the higher HAM-D and anxiety scale, the more reduced brain volume in limbic lobe and parietal lobe of MDD patients with and without suicidal ideation. We also found the volume difference between MDD patients with and without suicidal ideation was in temporal lobe, and the shape difference was in the thalamus, amygdala and hippocampus. The limbic system includes limbic lobe, hippocampus and amygdala, and involves in motivation, emotion, learning and memory. The previous study showed suicidal attempts in young depressed patients may be related to abnormal gray matter volumes in temporal–parietal–limbic networks 3. The previous study found the largest difference between MDD with and without suicidal ideation was observed in the amygdala 4. In addition, the previous study also showed that depressed suicide attempters have smaller hippocampus than depressed patients without suicide attempts 5.Conclusion
We found the negative correlation between the brain volume of limbic system in MDD patients. We also found the significantly difference in brain volume and shape of limbic system between suicidal ideation and non-suicidal ideation. The result pointed out the importance of suicidal ideation, and encourage to find out the solution for reducing the MDD patients with suicidal ideation.Acknowledgements
This study was supported by the research programs MOST106-2314-B-182-040-MY3 and MOST105-2314-B-182-028, which were sponsored by the Ministry of Science and Technology, Taipei, Taiwan. This work was also supported by the research program CLRPG6G0041, which was sponsored by the Health Information and Epidemiology Laboratory, Chang Gung Memorial Hospital, Chiayi, Taiwan.References
1. Doreen M, Denis P, Binod TC, et al. A diffusion tensor imaging study of suicide attempters. J Psychiatr Res. 2014 Apr; 51:60-67.
2. Thomas R, Erich S, Fabrizio E, Roland W, LadislavV, Konrad M. An fMRI study on mental pain and suicidal behavior. J Affect Disord. 2010 Oct; 126(1-2):321–5.
3. Hongjun P, Kai W, Jie L, Haochen Q, Shengwen G, Minyue C, Xiaoming W, Yangbo G, Yuling Y, Yuping N. Increased suicide attempts in young depressed patients with abnormal temporal–parietal–limbic gray matter volume. Journal of Affective Disorders. 2014 Aug;165:69-73.
4. Rentería ME, Schmaal L, Hibar DP, et al. Subcortical brain structure and suicidal behaviour in major depressive disorder: a meta-analysis from the ENIGMA-MDD working group. Transl Psychiatry. 2017 May; 7(5):e1116.
5. Romain C, Marie C, Claire C, ChristopheV, Florence G, Patrick H, Bruno F, Olivier C, Denis D, Emmanuelle C. Depressed suicide attempters have smaller hippocampus than depressed patients without suicide attempts. Journal of Psychiatric Research. 2015 Feb; 61:13-18.
Figures