1799
Quantification of Diffusion Tensor Imaging (DTI) in the Pediatric Spinal Cord: Application to Clinical Evaluation1Radiology, Vanderbilt Childrens’s Hospital, Nashville, TN, United States, 2Vanderbilt University Institute of Imaging Science, Nashville, TN, United States, 3Urology, Vanderbilt Childrens’s Hospital, Nashville, TN, United States, 4Neurosurgery, Vanderbilt Childrens’s Hospital, Nashville, TN, United States
Synopsis
The goal of the study was to apply optimized Diffusion Tensor Imaging (DTI) in the pediatric spinal cord and quantified to determine normative DTI-derived indices based on age. DTI was acquired in 35 patients, 22 being normal and AD, FA, MD, and RD were calculated.
DTI of the spinal cord in the pediatric population can be performed in the clinical setting to produce reliable DTI values. AD and MD demonstrated statistically significant changes based on age in both normal patients and the complete patient population.
Purpose:
The purpose of the study is to apply Diffusion Tensor Imaging (DTI) to the spinal cord (SC) in children. DTI of the SC is challenging with the anatomic size of the SC much smaller compared to the brain, and further challenging in children, where respiratory motion within the thoracic cord and patient motion in nonsedated cases can be problematic. We performed and quantified DTI indices: mean diffusivity (MD), axial diffusivity (AD), radial diffusivity (RD), and fractional anisotropy (FA) to determine normative DTI values and the relationship to age . This will help us further evaluate to future cases with spinal pathology such as tethered cord patients and post myelomeningocele repair patients.Methods:
A retrospective analysis was performed on DTI acquired as part of clinical MRI SC protocol in the pediatric population at Vanderbilt Children’s Hospital. Diffusion weighted images (15 directions, b=1000, slice thickness=5mm, nominal in-plane resolution=1.0x1.0mm) were acquired on a 3.0 T Philips Achieva in the cervical or thoracic/lumbar SC. Each DTI acquisition included 14 axial slices. Volumes of interest (VOI) were manually selected for each axial slice to include the entire cord and exclude CSF and conus. Slices with substantial artifacts were excluded. The mean DTI index was calculated across all voxels within the VOI, resulting in a single MD, AD, RD, and FA value for each subject’s cervical or thoracic/lumbar SC. These values were then correlated with the patients’ ages, using a linear regression. This correlation was performed for: 1) all patients regardless of diagnosis (all patients) and regardless of cord region, 2) all patients with cervical cord data, 3) all patients with thoracic/lumbar cord, 4) normal cord based on conventional MRI sequences but regardless of cord region, 5) normal patients with cervical cord data, and 6) normal patients with thoracic cord data. Demographics were: 22 normal patients (7 within the cervical SC and 15 in the thoracic/lumbar SC), 13 patients with pathologic cord (6 within the cervical SC and 7 in the thoracic/lumbar SC). The ages ranged from 4 months to 16 years old. Statistical analysis was performed with Pearson’s correlation to calculate p and r values.Results:
Figure 1 shows the linear regression results. Both AD and MD significantly correlated with age and increased over time in the cervical SC in both normal patients (n = 7; AD: R = 0.9, p = 0.005; MD: R = 0.9, p = 0.003), as well as in all patients (n = 13; AD: R = 0.8, p = 0.0005; MD: R = 0.6, p = 0.03) which include normal and pathological patients (Figure 1). FA appeared to increase with age within the cervical SC, but this trend was not statistically significant (Figure 2).Conclusion:
DTI of the SC in the pediatric population can be performed in the clinical setting to produce DTI reliable values. AD and MD demonstrated statistically significant changes based on age in both normal patients and the complete patient population which included normal and pathology. These findings need to be validated with a larger patient population and future studies to include specific spine pathologies, such as syrinx in Chiari I and tethered cord in post myelomeningocele repair patients. Currently there are no reliable imaging findings on conventional MRI to determine which patients need surgical intervention in Chiari I or truly have a tethered cord, DTI may potentially be a biomarker to help our clinical colleagues in neurosurgery, urology, and orthopedics.Acknowledgements
No acknowledgement found.References
No reference found.Figures
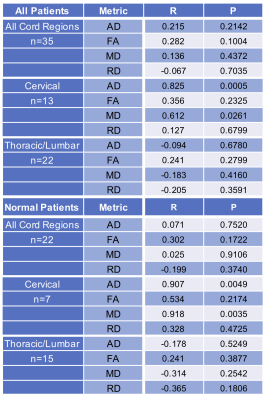
Figure 1. DTI data
DTI volumetric data including AD, FA, MD, and RD, displayed for all normal patients (n = 22), and separated into cervical cord (n = 7) and thoracic/lumbar cord (n = 15). The DTI values are also displayed for all patients (n = 35), which included normal and pathology, and separated into cervical cord (n = 13) and thoracic/lumbar cord (n = 22). Yellow highlighted cells depict statistical significance.
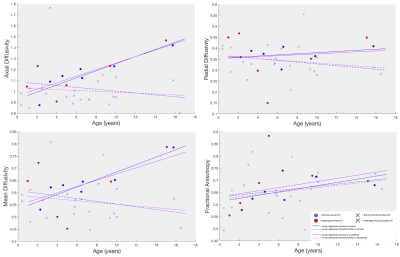
Figure 2. DTI value graphs
DTI volumetric values plotted vs age. Each data point is one patient. The normal patients are in blue and pathology in red, with solid circles representing cervical data and X’s representing lumbar/thoracic data. The lines are linear regression of the data, with solid lines for cervical and dashed for lumbar/thoracic. The blue lines represent normal and the purple lines are for all patients.