1657
Diffusion tensor MR imaging of optic radiation in advanced bilateral glaucoma patients in comparison to normal control subjects1Department of Radiology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand, 2Department of Radiological Technology, Faculty of Medical Technology, Mahidol University, Bangkok, Thailand, 3Department of Ophthalmology, Faculty of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand, 4Philips Healthcare, Singapore, Singapore
Synopsis
Glaucoma is a worldwide leading cause of irreversible vision loss characterized by degeneration of retinal ganglion cells. The damage can be found in visual pathway beyond retina and optic disc to visual cortex. Diffusion tensor MR imaging (DTI) is widely used for evaluation of early microstructural change in the brain parenchyma. Here we reported abnormal change of the optic radiation in advanced bilateral glaucoma patients using DTI as compared to the age-matched normal control subjects. The obtained DTI parameters may serve as potential quantitative imaging biomarkers to provide complementary indication of the disease condition in glaucoma.
Introduction
Glaucoma is a leading cause of irreversible vision loss, characterized by degeneration of retinal ganglion cells and resulting changes in optic disc or visual field defects 1. The abnormality can be found in visual pathway and visual cortex beyond retina and optic disc, although the pathophysiology of glaucomatous optic neuropathy is still not well understood. This study aimed to evaluate microstructural changes of the optic radiation in advanced bilateral glaucoma patients by applying diffusion tensor MR imaging (DTI) and to compare with normal subjects.Materials and Methods
All human subjects underwent MRI on a 3T system (Philips Ingenia). The protocol was approved by the local ethnic review board, and informed consent was obtained from each participant. Conventional clinical protocol included 3D T1-weighted and fluid-attenuated inversion recovery (FLAIR) imaging. For DTI a single-shot motion-sensitized spin-echo EPI sequence was used with 32 diffusion-encoding directions and one non-zero b-values (800 s/mm2) covering the whole brain. A high parallel imaging factor of 4 with sensitivity encoding (SENSE) was adopted to minimize EPI-associated susceptibility artifacts as well as geometric distortion. The typical imaging parameters were: field-of-view FOV 224 × 224 mm2, matrix size 112 × 112, voxel size 2 × 2 × 2 mm3, 70 contiguous slices; spectral presaturation with inversion recovery (SPIR) for fat suppression; repetition time TR / echo time TE 9422 to 9564 / 74 ms, EPI factor 27, 2 averages (NSA); scan time 12 min. The obtained images were processed for probabilistic tractography of the optic radiation (Figure 1) by using FSL software 2, seeding ROI (region of interest) from lateral geniculate nucleus (LGN) and terminating at V1 cortex (primary visual cortex) which created from standard space template. The derived DTI parameters including fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD) and radial diffusivities (RD) were compared. In addition, the glaucoma severity was clinically assessed with a six-stage system based on static threshold visual field parameters. Statistical analysis was done in SPSS and a P value <0.01 was considered significant.Results
In total 10 patients with bilateral advanced bilateral glaucoma (mean age 62 years and range 43-73 years, 5 males) and 10 age-matched normal subjects (mean age 60 years and range 44-80 years, 4 males) as control were scanned. Fiber tracking was successful in all subjects based on the obtained diffusion images. In general, visual appearance of b0 and b800 images showed no obvious difference between patients and normal subjects. Derived fiber tractography overlaid to FA maps showed clearly thinning of the fiber tract in optic radiation in patients compared to normal subjects (Figure 1). Two sets of probabilistic threshold for fiber tractography were tested and evaluated in both patients and normal controls, namely 300 and 500 connectivity per voxel 3. A systematic evaluation revealed that the FA of optic radiations in glaucoma patients was statistically significantly decreased (p<0.01), whereas MD, AD and RD were statistically significantly increased in glaucoma patients as compared with normal control subjects (p<0.01), in agreement to the previous report 4. Details were summarized in Table 1. A threshold of 500 fibers per voxel showed higher FA and lower RD in both patient and control groups (P<0.05), while no statistically significant difference in MD and AD.Discussion and Conclusion:
Despite relatively small sample size, we have demonstrated an abnormal change and an extended damage of the optic radiation in advanced bilateral glaucoma patients by using DTI, possibly due to transsynaptic degeneration process. Derived parameters of diffusion property may provide complementary indication of glaucoma disease severity but this still need further clinical studies in a larger cohort.Acknowledgements
This research project was supported by Faculty of Medicine Siriraj Hospital, Mahidol University, Grant Number R015832032.References
1. Gupta N, Yucel YH. Curr Opin Ophthalmol 2007;18:110.
2. Jenkinson M, et al. NeuroImage 2012;62:782.
3. Behrens TEJ, et al. NeuroImage 2007;23:144.
4. Dai H, et al. Neuroradiololgy 2013;55:233.
Figures

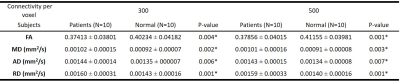
Table 1. DTI of optic radiations in the advanced glaucoma patients and normal control groups. Data were reported in means ± standard deviation (SD).
* Statistical significance; FA, fractional anisotropy; MD, mean diffusivity; AD, axial diffusivity; RD, radial diffusivity.