1522
Brain metastases developing pseudoprogression have poor vascular function and supply1Department of Diagnostic Physics, Oslo University Hospital, Oslo, Norway, 2Department of Radiology and Nuclear Medicine, Oslo University Hospital, Oslo, Norway, 3Department of Radiology, Østfold Hospital Trust, Kalnes, Norway, 4Deptartment of Radiology, Hospital of Southern Norway, Kristiansand, Norway, 5Department of Oncology, Oslo University Hospital, Oslo, Norway
Synopsis
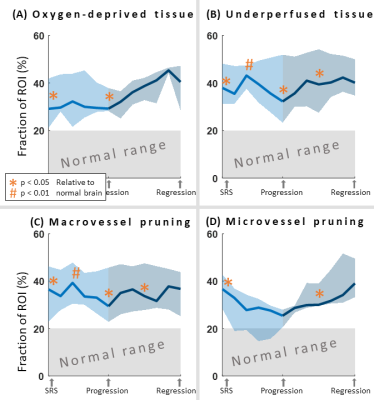
Stereotactic radiosurgery of brain metastases can cause pseudoprogression. In this study, we use Vessel Architectural Imaging, based on dual echo DSC, to investigate the course of vascular function of brain metastases, both prior to and after pseudoprogression have occurred. Our results show that pseudoprogressing metastases were characterized by underperfused and oxygen-deprived tissue, and micro- and macrovessel pruning in the peritumoral regions. This was in contrast to peritumoral regions of responding metastases as well as normal-appearing brain tissue.
Introduction
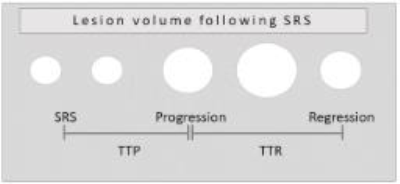
Stereotactic radiosurgery (SRS) is an important treatment option for patients with brain metastases. However, SRS can cause pseudoprogression, a radiation-induced tissue damage which leads to a transient increase with subsequently decrease of the lesion volume on post-gadolinium T1-weighted images. The time from SRS to an apparent tumor volume increase, i.e. pseudoprogression (TTP), and the time from pseudoprogression to subsequent manifested regression (TTR) can vary from a few months and up to years1 (Figure 1). Studies of pseudoprogression using perfusion Magnetic Resonance Imaging (MRI) to understand the mechanisms of pseudoprogression are mainly limited to one follow-up exam or only after the occurrence of pseudoprogression. Here, we use Vessel Architectural Imaging (VAI)2 to investigate the course of vascular function of brain metastases, prior to and after pseudoprogression have occurred.Methods
Seventeen patients with 19 metastases from non-small cell lung cancer or malignant melanoma received SRS (15-25 Gy) to the metastases + 2mm margin. MRI, including dual echo dynamic susceptibility contrast (DSC) imaging, was acquired pre-SRS, every 3 months the first year and every 6 months thereafter. Seven patients with 8 metastases were classified as pseudoprogression based on follow-up or histology. DSC and VAI data enabled measures of oxygenation status, as well as micro- and macrovascular blood volume, blood flow and vessel calibers.3 Peritumoral region were defined by a 4mm wide dilation around the enhancing lesion. Fractions of deviant vascular characteristics in peritumoral region were calculated based on the number of voxels with parameter values under/above the 20th/80th percentile of the normal-appearing brain tissue. Longitudinal data from pseudoprogressing metastases was normalized to pre-SRS, TTP and TTR.Results
Median TTP was 6 months (range: 3 – 18 months) and subsequent median TTR occurred at 6 months (range: 3 - 17 months). The peritumoral region of pseudoprogressing metastases were characterized by underperfused and oxygen-deprived tissue, and micro- and macrovessel pruning, both prior to and after SRS (p < 0.05, relative to normal-appearing brain) (Figure 2A-D). In responding metastases, by contrast, no difference between peritumoral regions and normal brain was found. Moreover, a trend towards increased fraction of oxygen-deprived tissue and microvessel pruning were observed after the manifestation of pseudoprogression on post-gadolinium T1-weighted images.Discussion and Conclusion
Our findings show that metastases developing pseudoprogression are characterized by poor vascular function in the peritumoral region compared to responding metastases and normal-appearing brain tissue. The increase in fraction of oxygen-deprived tissue after the manifestation of pseudoprogression are in line with histological findings showing hypoxia-inducible factors in tissue with pseudoprogression.4 Combined, our data provide valuable and novel insight into the vascular function in SRS-treated metastases developing pseudoprogression.Acknowledgements
No acknowledgement found.References
1. Parvez K et al. Int J Mol Sci. 2014;15:11832-11846.
2. Emblem KE et al. Nat Med. 2013;19(9):1178-83
3. Digernes I et al. J Cereb Blood Flow Metab. 2017;37(6):2237-2248
4. Nonoguchi et al. J Neurooncol. 2011;105:423-431.
Figures