1460
The effect of fetal dielectric properties, position and blood-flow in maternal tissues on fetal temperature for fetal MRI at 3T1School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom
Synopsis
Effects of age adjusted dielectric properties for fetal tissues compared to adult values, fetal position, and blood-flow in maternal tissues on fetal temperature in a model of a 7 month pregnant woman within a 3T birdcage coil were investigated numerically. Age adjusted properties resulted in small increases in peak and mean fetal temperatures and reduced time to reach a peak fetal temperature of 39°C. Changes in fetal position produced a greater effect on peak and mean fetal temperatures. Temperature dependent blood-flow in maternal superficial tissues had little effect on fetal temperature.
Purpose
To investigate the effect of (a) the higher water content of fetal tissues compared to adult tissues on dielectric properties and hence interaction of the RF field, (b) fetal position on fetal heating during MR fetal imaging and (c) effect of temperature dependence of maternal blood-flow on fetal temperature.Methods
A pregnant woman model1 was positioned fetal heart centred within a 600 mm diameter, 400 mm long band-pass, shielded 127 MHz coil which was excited in quadrature. RF fields and resulting temperatures were calculated using Sim4Life v3.4.1 software (Zurich Med Tech). Maternal tissue properties were taken from a standard database2 and temperature dependence of maternal skin, fat and muscle blood-flow were treated as in Murbach et al3. Age adjusted dielectric properties of fetal tissues, accounting for their higher water content compared with adult ones, were estimated using the approach reported by Wang et al4 as previously reported5. Thermal properties of fetal tissues were assumed to be those of adult tissues with temperature independent blood-flow. Five cases were investigated in which fetal dielectric properties, maternal blood-flow, and fetal position were varied (see caption to Table 1). It is important that realistic properties6 (ε=76, s=1.25 S/m), rather than a surrogate (e.g. cerebrospinal fluid (2.14 S/m)2), are given to amniotic fluid when assessing fetal exposure during MRI5. The equilibrium temperature distribution (zero RF power) was simulated and then used as the initial conditions for simulating temperature changes over 60min at the RF power level resulting in a maternal whole body SAR of 2 W/kg.Results
Table 1 contains temperature data; Figure 2 shows the time-course profiles for case 1. Since temperature may reach a steady-state in excess of guideline limits, we also quote ‘time to 39°C’ – i.e. the period of 2W/kg exposure that can be tolerated before violating the limit associated with normal mode operation7. Figure 3 shows pairwise comparisons. Case1 vs Case2 suggests a modest increase in maximum fetal temperature of ~0.2°C results from use of age adjusted fetal properties. The increase in the mean fetal temperature after 60min of applied RF was marginally above/below the recommended limit7 (0.5°C) when age adjusted/adult properties, respectively, were assumed. Although temperature dependent blood-flow in maternal superficial tissues resulted in a 1.9°C decrease in the peak temperature in the maternal trunk in Case1 compared to Case3, this difference in modelling maternal blood-flow had a smaller effect on fetal temperatures. Comparison of maximum temperatures observed when the fetus was head down or head up (Case1 v Case4) suggests up to ~0.2°C difference in peak temperature. Rotation of the fetus 20 degrees around its long axis (Case5) resulted in the greatest deviation from Case1 with the smallest increase in both peak and mean fetal temperatures in the examples investigated and 45mins to reach 39°C. Figure 4 shows that the hotspot in the mother is usually in the pelvis, away from the fetus.Discussion
Use of age adjusted dielectric properties for fetal tissues leads to modest increases in peak and mean fetal temperatures. However, the increase in peak temperature results in a significant shortening of the time to 39°C. Temperature dependence of blood-flow in superficial maternal tissues is important in predicting maternal tissue temperatures but has little effect on fetal temperatures. We have also investigated the effect of assuming (unrealistically) that all maternal tissues have a temperature dependence similar to that of skin3 and found the peak fetal temperature is only 0.05°C lower than values reported here. When the fetus is in the head up position only a small increase in peak fetal temperature of up to 0.2oC compared to the original head down position is predicted. In these two positions the fetus occupies essentially the same spatial volume. However when the fetus is rotated 20 degrees about the long axis, occupying a different spatial volume, the peak fetal temperature is up to 0.5oC lower than that for the non-rotated case and the 39oC limit7 is reached only after 45mins exposure.Conclusion
Accounting for the higher water content of fetal tissues (compared to adult tissues) in simulations of fetal exposure during MR imaging results in a modest increase in predicted peak and mean fetal temperatures. This study suggests that changes in fetal position may have a greater effect on fetal temperature. There is a need to investigate the effect of time varying, realistic fetal movement on fetal temperature to improve assessment of the effect of RF exposure on fetal safety.Acknowledgements
This work was supported by the Wellcome EPSRC Centre for Medical Engineering at Kings College London (WT 203148/Z/16/Z), MRC strategic grant MR/K006355/1, EPSRC fellowship award (EP/L00531X/1) and by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.References
- Gosselin, M.C. Neufeld E, Moser H, et al. Development of a new generation of high-resolution anatomical models for medical device evaluation: the Virtual Population 3.0. Phys Med Biol. 2014;59:5287–5303.
- Hasgall PA, Di Gennaro F, Baumgartner C, et al. IT’IS Database for thermal and electromagnetic parameters of biological tissues, Version 3.0. (2015) DOI: 10.13099/VIP21000-03-0.
- Murbach M, Neufeld E, Theodoros Samaras T, et al. Pregnant women models analyzed for RF exposure and temperature increase in 3T RF shimmed birdcages. Magn Reson Med. 2017;77:2048–2056.
- Wang J, Fujiwara O, Watanabe S. Approximation of aging effect on dielectric tissue properties for SAR assessment of mobile telephones. IEEE Trans. Electromagn. Compat. 2006;48:408–413.
- Malik SJ, Hand JW, Hajnal JV. The effect of variable amniotic fluid conductivity and fetal tissues properties on B1+ and local SAR for fetal imaging at 3T. Proc. Intl. Soc. Magn. Reson. Med. 2017;25: 5578
- Peyman A, Gabriel C, Benedickter HR, Frohlich J. Dielectric properties of human placenta, umbilical cord and amniotic fluid. Phys. Med. Biol. 2011;56:93-98.
- IEC 60601-2-33:2010+A1 Medical electrical equipment Part 2-33: Particular requirements for the basic safety and essential performance of magnetic resonance equipment for medical diagnosis. International Electrotechnical Commission. 2015
Figures
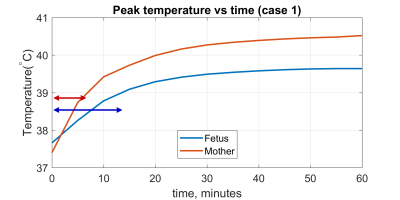
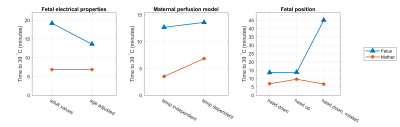
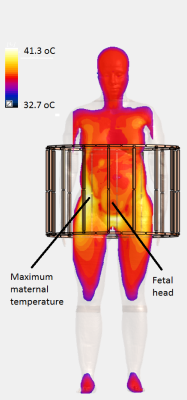
Table 1. Fetal peak and mean temperatures for the 5 cases studied.
Case 1: head down, age adjusted fetal dielectric properties, temperature dependent maternal blood-flow.
Case 2: head down, adult values for fetal dielectric properties, temperature dependent maternal blood-flow.
Case 3: head down, age adjusted fetal dielectric properties, temperature independent maternal blood-flow.
Case 4: head up, age adjusted fetal dielectric properties, temperature dependent maternal blood-flow.
Case 5: head down, rotation of 20 degrees around the long axis of the fetus, age adjusted fetal dielectric properties, temperature dependent maternal blood-flow.