1429
Impact of Respiratory Triggering in 3T Sub-Millimeter High Resolution Brachial Plexus MRIDarryl B Sneag1, Jacqui C Zhu1, Susan Lee1, Tina Jeon1, Bin Lin1, and Maggie M Fung2
1Radiology, Hospital of Special Surgery, New York, NY, United States, 2Applications & Workflow, GE Healthcare, New York, NY, United States
Synopsis
This study’s purpose was to compare non-respiratory and respiratory- triggered proton density and T2-weighted DIXON fat suppression sequences for high-resolution brachial plexus MRI. In a cohort of 5 volunteers and 20 patients, we were able to demonstrate that respiratory triggering substantially reduced ghosting artifact and improved delineation of nerve fascicular architecture with acceptable increased scan time.
Purpose
Oblique sagittal high resolution MRI sequences, orthogonal to the longitudinal axis of the brachial plexus, can reliably depict morphologic and signal abnormalities. However, this acquisition technique can be challenging due to respiratory-induced ghosting artifact that may obscure nerve detail. More than two decades ago, Posniak et al. mentioned the possible use of respiratory triggering (RT) for plexus MRI1. However, the efficacy of RT for brachial plexus imaging has not yet been reported. Our hypothesis was that RT would minimize ghosting artifact and improve nerve conspicuity of the brachial plexus, without prohibitive scan time penalty.Methods
In this prospective, IRB-approved study of 5 healthy volunteers and 20 patients, proton density (PD) or T2-weighted Dixon fat suppressed (DFS) sequences with and without RT (with the same scan coverage and comparable spatial resolution – Table 1), were acquired consecutively within each examination. The study was performed on three 3T 60cm bore scanners (Discovery MR750, GE Healthcare, USA) using 16 channel small and/or medium flexible coils. RT was achieved prospectively with a thoracic bellow, 1-2 respiratory rate (RR) intervals, trigger window = 40%, and trigger point = 30%. Two musculoskeletal radiologists, blinded to the presence of RT, scored the sequences independently. To optimize blinding, the non-RT and RT acquisitions of different subjects were submitted for scoring in a random fashion. Subjective scoring criteria for A) Ghosting artifact; B) Nerve conspicuity (defined as delineation of nerve fascicular architecture) for three regions of the brachial plexus (supraclavicular, retroclavicular and infraclavicular); and C) Overall diagnostic confidence were employed (Table 2). The total image quality score was computed by summing the scores of the three regions of B. RR, total scan time and number of slices were recorded, with average scan time per slice calculated. Wilcoxon signed-rank test was used to compare non-RT and RT parameters. Inter-observer agreement was assessed using weighted Cohen’s kappa analysis with the exception of total image quality score, which were evaluated with Krippendorf’s alpha analysis. Spearman correlation evaluated the associations of image quality with scan time and RR, where good image quality defined by nerve conspicuity score ≥3 (Scale 1- 4, Table 2). Significance was set a priori to p<0.05.Results
In 25 subjects, 50 sequences were compared (4 PD, 12 3-pt. DFS, 34 2-pt. DFS). Figure 1 shows the subjective scoring comparison results. RT demonstrated improvements in all image quality catergories with statistical significance (p<0.05). The diagnostic confidence increased for both readers from a median score of 2 to 3 ( p = 0.02 for reader 1 and p = 0.04 for reader 2). Inter-observer agreement for asessment of ghosting artifact showed substantial to almost perfect agreement (kappa coefficents: 0.81 for non-RT and 0.77 for RT). Evaluation of nerve conspicuity demonstrated almost perfect agreement (Krippendorff's alpha coefficients: 0.986 for non-RT and 0.985 for RT). Inter-observer agreement of the remaining scores demonstrated moderate to substantial agreement (kappa coefficient ranging from: 0.41-0.79). There was no evidence of association between scan time with good image quality on non-RT or RT sequences (Spearman’s ρ ranging from: -0.35 to 0.29 and -0.04 to 0.29 respectively). There was a consistent weakly positive correlation between higher respiratory rate and good image quality (Spearman’s ρ ranging from: 0.28-0.43). Median scan time per slice increased from 6.95 sec (non-RT) to 10.21 sec (RT) (46% increase) and total median scan time increased from 4:44 min. (non-RT) to 6:00 min. (RT) (36% increase).Discussion
This study demonstrated that for brachial plexus MRI, RT can reduce ghosting artifact, improve nerve fascicular architecture delineation and increase overall diagnostic confidence, with acceptable scan time cost and very good inter-observer agreement. There was a consistent weak association between higher respiratory rate and better image quality. A lower respiratory rate was challenging for RT scans as all slices in a respiratory cycle are acquired in a single TR, thereby contributing to a relatively long non-data filling period. An additional challenge we subjectively observed with respiratory triggering was an irregular respiratory rhythm, which occasionally precipitated imperfect triggering. RT techniques that better incorporate RR and respiratory rhythm may further minimize scan time and improve image quality.Conclusion
Given the acceptable scan time impact observed in this study, use of RT could be considered for high resolution brachial plexus MRI to minimize artifact and improve image quality. Alternative techniques, such as soft gating3,4 or guided breathing that are insensitive to respiratory patterns may be further investigated to mitigate artifact.Acknowledgements
Hospital of Special Surgery has an institutional agreement with GE HealthcareReferences
[1] Posniak, H et al. MR Imaging of the Brachial Plexus. American Journal of Radiology 1993: 161; 373-379. [2] Cheng JY, et al. JMRI 2014, [3] Lai, ISMRM, 2017
Figures
Table 1. Imaging Parameters
Table 2. Subjective scoring criteria
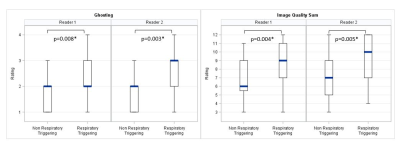
Figure 1. Box-plot depiction
demonstrating scoring comparisons
between non
respiratory trigger and respiratory sequences for the two readers. Respiratory triggering
reduced ghosting artifact and improved image quality.
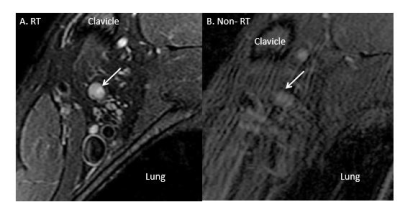
Figure 2. Oblique sagittal T2-weighted
Dixon fat suppression images. Image A
with respiratory triggering clearly
demonstrates a nerve sheath tumor (arrow) arising from
the posterior
division of the superior trunk, which is nearly inconspicuous on the image B
without respiratory triggering.
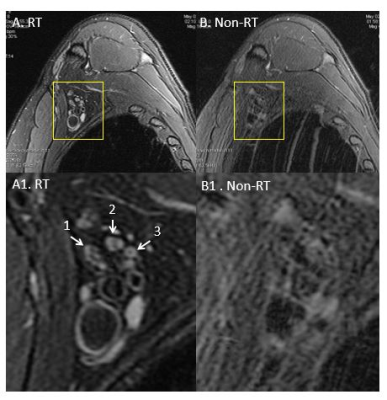
Figure 3. Oblique sagittal T2-weighted Dixon fat
suppression images. Images
A1 and A2 with respiratory triggering show clear delineation of nerve
fascicular architecture, which is markedly blurred on images B1 and B2 without
respiratory triggering. Arrow 1, 2 and 3 denotes lateral cord, posterior cord
and medial cord of the brachial plexus respectively.