1419
3D high resolution MR imaging of anterolateral ligament1The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, 2Clinical Science, Philips Healthcare, Beijing, China
Synopsis
This study aimed to demonstrate the feasibility of optimized 3D high resolution MR imaging for scanning anterolaterl ligament, as well as provide more accurate imaging technique for patient with ACL and ALL injured. In the study, we used the high resolution 3D TSE-based sequences including the optimized T1W-VISTA, PDW-VISTA, and T1W-VISTA-SPAIR to evaluate the 60 knees of thirty healthy volunteers. There was significant difference between the three techniques for both the radiologists, and there was high consistency between the scores of two radiologists. 3D T1W-VISTA imaging technique has a high superiority in the three techniques, which may provide more information for clinical diagnosis.
Purpose
Recent studies have characterized the anterolateral ligament (ALL) of the knee in detail. This structure is regarded as having a complementary function to the anterior cruciate ligament (ACL) which keeps anterolateral rotational knee stability. The association of ALL injuries with ACL ruptures would cause for anterolateral rotatory instability. Recently studies have evaluated the structure of ALL by using routine MRI techniques. However, the ALL is a relatively thin ligament. The routine MRI imaging can only showed a part of the ALL rather than the whole ligament anatomy or its adjacent relations. This study attempts to optimize the high resolution 3D MR imaging to show a better understand the structural characteristics of ALL.Methods
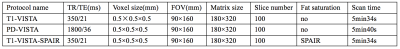
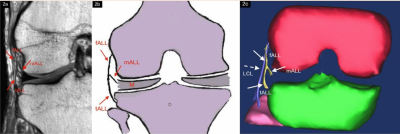
Thirty volunteers (18 males, 12 females, aged 31.2±5.6 years old) who have no history of knee injury and surgery and no knee pains were included. All MRI scans were performed on a 3.0T MR scanner (Ingenia, Philips Healthcare, Best, the Netherlands) using a dedicated 8-channel knee coil. Both the left and right knees were scanned respectively. The high resolution 3D TSE-based sequences including the T1W-VISTA, PDW-VISTA, and T1W-VISTA-SPAIR were optimized for the scanning.Totally 60 knees were imaged divided into femoral portion, meniscal portion, and tibial portion for analyses. Two musculoskeletal radiologists with more than 5 years experience were blinded to evaluate the image quality of ALL separately. Five grades as follows: grade0, the image quality is poor and is not conducive for clinical diagnosis; grade1, only one part of ALL can be visualized, the contrast with the surrounding soft tissue is poor, the resolution and SNR is low; grade2, only parts of ALL can be visualized, the contrast or resolution or SNR is good; grade3, whole of ALL can be visualized, the contrast or resolution or SNR is good; grade4, whole ALL can be visualized, the contrast, resolution and SNR are all good.The knees were then dissected on the clearest sequence to assess the visibility of each part of ALL. Kruskal-Wallis test was used to compare the difference of the images of the three techniques for both the radiologists. Kappa test was used to compare the evaluation consistency of the two radiologists. A 3D reconstruction of the ALL was carried out by using Mimics software (Release 15.0).Result:
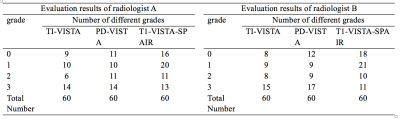
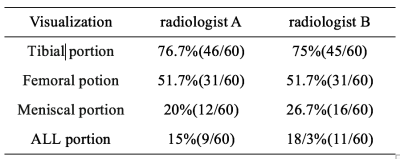
The evaluation results of radiologist A:for the percent of 3 or 4 scores , 67.5% for T1-VISTA, and only 20% for T1-VISTA-SPAIR .And there are significant difference (χ2=19.53,p<0.05). The evaluation results of radiologist B:for the percent of 3 or 4 image scores, 67.5% for T1-VISTA,and only 15% for T1-VISTA-SPAIR. And there are significant difference (χ2=26.52,p<0.05). The consistency coefficient is 0.761 for T1-VISTA, 0.777 for PD-VISTA and 0.645 for T1-VISTA-SPAIR respectively, which show that there was high consistency between the two radiologists. T1W-VISTA imaging technique has a high superiority in the imaging of the ALL.The tibial portion was mostly visualized (76.6 % of radiologists A,75 % of radiologists B), followed by the femoral portion (51.7 % of radiologists A and B) and the meniscal portions(20 % of radiologists A26.7 % of radiologists B). The entire paths of all three ligament portions were visualized with only 15% of radiologists A and 18.3% of radiologists B. T1-VISTA-SPAIR sequence is helpful to show the relationship between ALL and ACL injured.Discussion
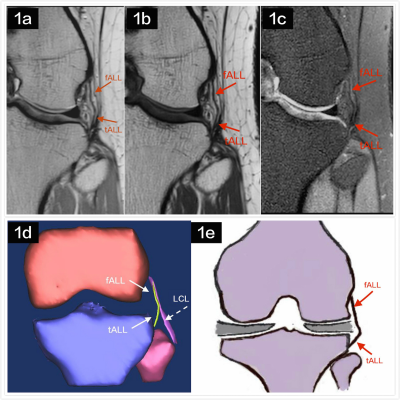
The ALL is described as a distinct ligamentous structure, originating from the prominence of lateral femoral epicondyle anterior to the attachment of the lateral collateral ligament, with an oblique course, inserting on the tibial plateau and in some case can into the lateral meniscus.The 3D T1W-VISTA sequence has the best performance in the anatomical of ALL imaging. For T1W-VISTA, contrast with the surrounding tissue was more obvious, which can clearly show the originates, attachments and trajectory of ALL. The reconstruction of the ALL by using T1-VISTA images can clearly identify the whole structure of ALL which can provide a better understanding of the ligament structure and the relationship with surrounding structures. In addition, T1-VISTA imaging is feasible in clinical within a scanning time of 5min34s.When the ligament injured, the ligament itself, the surrounding soft tissue are usually edema, then the ligament will be difficult to be observed. In this case, the T1-VISTA-SPAIR sequence with fat suppression should be scanned, which increases the contrast to the surrounding tissue and display the damages caused by edema, which is helpful to find the potential relationship between the ACL and ALL.Conclusion
3D T1W-VISTA imaging has a high superiority in the imaging of the ALL.The tibial portion being the most clearly visualized and the meniscal portion the least clearly visualized. When the knee injured, the T1-VISTA-SPAIR sequence might be helpful to show the relationship between ALL damage and ACL damage.Acknowledgements
No acknowledgement found.References
[1] Parsons EM, Gee AO, Spiekerman C,et al. The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med. 2015;43(3):669-74.
[2] Spencer L, Burkhart TA, Tran MN,et al. Biomechanical analysis of simulated clinical testing and reconstruction of theanterolateral ligament of the knee. Am J Sports Med. 2015;43(9):2189-97.
Figures