1415
Cartilage and Meniscus T2 Relaxation Time in Subjects With and Without Meniscus Tears1Department of Radiology, University of Wisconsin-Madison, Madison, WI, United States
Synopsis
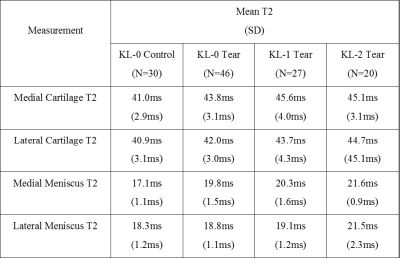
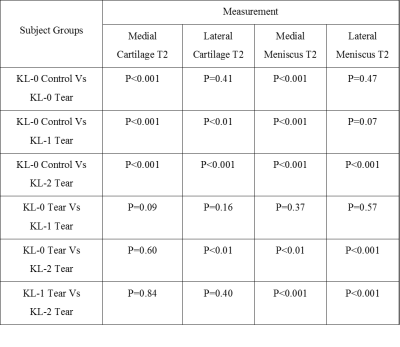
This study was performed to compare cartilage T2 between subjects with and without meniscus tears. T2 mapping was performed on the knees of 30 control subjects without meniscus tears and 93 subjects with meniscus tears. Medial and lateral compartment cartilage T2 was measured. Radiographic osteoarthritis severity was assessed using the Kellgren-Lawrence (KL) grading scale. The 30 KL-0 control subjects without meniscus tears had significantly lower (p<0.001) medial compartment cartilage T2 than KL-0 (n=46), KL 1 (n=27), and KL-2 (n=20) subjects with meniscus tears and significantly lower (p<0.01) lateral compartment cartilage T2 than KL-1 and KL-2 subjects with meniscus tears.
Introduction
Previous studies using quantitative magnetic resonance imaging (MRI) to investigate the association between meniscus tears and knee joint cartilage degeneration have been limited by small subject populations [1, 2], combining individuals with varying degrees of osteoarthritis (OA) into subject groups with and without meniscus tears [1-4], and measuring MRI parameters in small regions of interest (ROIs) within cartilage [3, 4]. This study was performed to compare medial and lateral compartment cartilage T2 relaxation time between a control group of subjects without meniscus tears or knee OA and three individual groups of subjects with meniscus tears and varying degrees of knee OA.Methods
A multi-echo spin-echo T2 mapping sequence (Cartigram, GE Healthcare) was performed on the knees of 93 subjects with tears of the posterior horn of the medial and/or lateral meniscus identified at knee arthroscopy and a control group of 30 subjects without meniscus tears or knee OA. No subjects had associated ligament injuries or bone contusions on MRI or arthroscopy. Images were acquired using a 3T scanner (Sigma Excite HDx, GE Healthcare) and 8-channel extremity coil with TR=1500ms, TE=9,18, 25, 36, 43, 55, 62, and 71ms, 90o flip angle, 16cm field of view, 256 x 192 matrix, 3mm slice thickness, and one signal average. T2 maps were created in MATLAB using a mono-exponential fitting method utilizing all 8 echoes for cartilage and the first 6 echoes for meniscus. ROIs were placed on meniscus and cartilage on each image slice to measure the mean T2 of the entire medial and lateral meniscus and the mean cartilage T2 in the entire medial compartment (medial femoral condyle and media tibia plateau) and lateral compartment (lateral femoral condyle and lateral tibia plateau). Radiographs were reviewed to determine the severity of knee OA using the Kellgren-Lawrence grading scale (KL-0=no OA, KL-1=minimal OA, KL-2=established OA) [5]. Meniscus tear type (vertical, horizontal, complex, or root) was documented at arthroscopy. Linear regression models adjusted for age and gender were used to compare cartilage and meniscus T2 between groups of subjects and to determine the association between cartilage and meniscus T2 and between cartilage T2 and meniscus tear type within the same compartment.Results
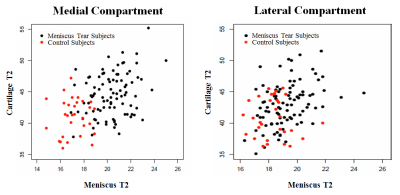
There were 87 subjects with medial meniscus tears and 27 subjects with lateral meniscus tears. The 30 KL-0 control subjects without meniscus tears had significantly lower (p<0.001) medial compartment cartilage T2 and medial meniscus T2 than KL-0 (n=46), KL 1 (n=27), and KL-2 (n=20) subjects with meniscus tears. The control subjects had significantly lower (p<0.01) lateral compartment cartilage T2 than KL-1 and KL-2 subjects with meniscus tears and significantly lower (p<0.001) lateral meniscus T2 than KL-2 subjects with meniscus tears (Figures 1 and 2). Control subjects had significantly lower (p<0.001) medial compartment cartilage T2 than 44 KL-0 subjects with medial meniscus tears, while there was no significant difference (p=0.80) in lateral compartment cartilage T2 between control subjects and 11 KL-0 subjects with lateral meniscus tears. There was no statistical difference (p=0.09-0.84) in cartilage T2 between KL-0, KL-1, or KL-2 subjects with meniscus tears except for a significantly higher (p<0.01) lateral compartment cartilage T2 in KL-0 subjects compared to KL-2 subjects. However, KL-0 subjects with meniscus tears had significantly lower (p<0.001) medial and lateral meniscus T2 than KL-1 and KL-2 subjects with meniscus tears (Figures 1 and 2). Cartilage T2 in the same compartment as the meniscus tear was not significantly different (p=0.06-0.81) between meniscus tear types. There was a significant association (p<0.01) between cartilage and meniscus T2 within the same compartment (Figure 3).Discussion
Our study has documented the presence of increased cartilage T2 in subjects with meniscus tears when compared to subjects without meniscus tears using experimental design and statistical analysis to account for potential confounding factors of age, gender, associated joint injuries, and KL grade. In fact, the difference in cartilage T2 in the medial and lateral compartments was much greater between subjects with and without meniscus tears than between subjects with meniscus tears who had different KL grades. There was a stronger association between meniscus tear and cartilage T2 for the medial compartment than the lateral compartment due to the relatively small number of subjects with lateral meniscus tears which greatly reduced statistical power. The strong direct correlation between cartilage and meniscus T2 in the same compartment and the significantly higher meniscus T2 in subjects with meniscus tears and higher KL grades reflects the important inter-relationship between changes in cartilage and meniscus during knee joint degeneration.Conclusion
Meniscus tears are an independent risk factor for early knee joint cartilage degeneration.Acknowledgements
We acknowledge support from NIH R01-AR068373-01, GE Healthcare, University of Wisconsin School of Medicine Shapiro Student Research Fellowship Program, and University of Wisconsin Department of Radiology Research and Development Committee.References
[1] K.M. Friedrich, T. Shepard, V.S. de Oliveira, L. Wang, J.S. Babb, M. Schweitzer, R. Regatte, T2 measurements of cartilage in osteoarthritis patients with meniscal tears, AJR. American journal of roentgenology, 193 (2009) W411-415.
[2] D. Kumar, J. Schooler, J. Zuo, C.E. McCulloch, L. Nardo, T.M. Link, X. Li, S. Majumdar, Trabecular bone structure and spatial differences in articular cartilage MR relaxation times in individuals with posterior horn medial meniscal tears, Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society, 21 (2013) 86-93.
[3] B. Kai, S.A. Mann, C. King, B.B. Forster, Integrity of articular cartilage on T2 mapping associated with meniscal signal change, European journal of radiology, 79 (2011) 421-427.
[4] K. Takahashi, S. Hashimoto, H. Nakamura, A. Mori, A. Sato, T. Majima, S. Takai, Medial meniscal posterior root/horn radial tears correlate with cartilage degeneration detected by T1rho relaxation mapping, European journal of radiology, 84 (2015) 1098-1104.
[5] J.H. Kellgren, J.S. Lawrence, Radiological assessment of osteo-arthrosis, Annals of the rheumatic diseases, 16 (1957) 494-502.
Figures