1412
A Prospective, Longitudinal Assessment of Adverse Local Tissue Reactions in Resurfacing Hip Arthroplasty Versus Primary Total Hip Arthroplasty1Hospital for Special Surgery, New York, NY, United States
Synopsis
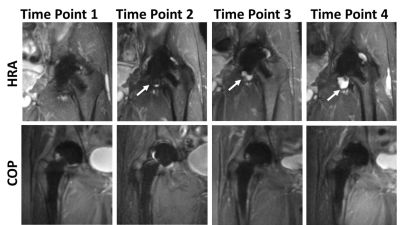
The purpose of this prospective study was to compare the prevalence of magnetic resonance imaging detected adverse local tissue reactions (ALTRs) in metal-on-metal hip resurfacing arthroplasty (HRA) and ceramic-on-poly (COP) total hip arthroplasty subjects. Images acquired at 4 time points with a 1-year interval showed a higher prevalence of ALTRs in the HRA than COP subjects. The self-assessed symptomatology scores did not significantly differ between the two groups at follow-up, indicating that ATLRs can be clinically silent. This study will permit better understanding of the natural history and follow up of ALTRs complicating hip arthroplasty.
Introduction
Failure of metal on metal (MOM) total hip arthroplasty (THA) and resurfacing arthroplasty (HRA) due to development of adverse local tissue reaction (ALTRs) is a significant clinical problem.1-3 The prevalence of ALTRs in asymptomatic MOM hip arthroplasty patients is highly variable, with rates reported from 5% to 68%.1-3 The purpose of this prospective longitudinal study was to: 1) determine ALTR prevalence in patients with MOM HRA; 2) determine if patients with HRA have a greater rate of ALTRs compared to control patients with ceramic on poly (COP) THA and 3) evaluate changes in patient reported outcomes in these two types of implant designs. We hypothesized that patients with HRA would have a greater prevalence of ALTRs.Methods
Following IRB approval with informed consent, primary COP and HRA patients who were at least one year post arthroplasty were enrolled and evaluated with annual MRIs. MRI was performed using clinical 1.5T scanners (GE Healthcare, Waukesha, WI) and 8 channel cardiac coils (Invivo, Gainesville, FL). Morphologic and susceptibility reduced images were acquired for each hip 4,5 and images were evaluated for the presence of synovitis, including synovial thickness and volume, and presence of ALTR.2,6 Patient reported outcomes were evaluated by Hip Disability and Osteoarthritis Outcome Scores (HOOS).7 Statistical analysis included: 1) Wilcoxon Rank Sum test to detect differences of age and LOI; 2) Chi-squared test to determine differences in gender distribution between COP and HRA subjects; 3) mixed-effects modeling to compare synovial thickness, synovial volume, and HOOS subgroups between bearing surfaces at each time point and within each bearing surface over time and 4) log-rank test and Cox proportional hazards modeling to compare the time to and the risk of developing ALTR between bearing surfaces. All models were adjusted for age, gender, and length of implantation. Significance is set at p<0.05. (SAS v9.4, Cary, NC).Results
A total of 83 subjects (83 hips) were evaluated at the initial time point (TP1): HRA, n=38, age=58.1±7.2 y.o., 31/7 (M/F), median LOI = 3.6 yr; COP, n=45, age=65.4±9.1 y.o., 22/23 (M/F), median LOI = 2.3 yr. 73 subjects were evaluated at a second time point (TP2): HRA, n=36, median LOI=3.6 yr; COP, n=37, median LOI=2.3 yr. 55 subjects were evaluated at a third time point (TP3): HRA, n= 24, median LOI=3.2 yr; COP, n=31, median LOI=3 yr. 25 subjects were evaluated at a fourth time point (TP4): HRA, n=11, median LOI=3.4 yr; COP, n=14, median LOI=2.1 yr. The mean synovial volume of the HRA and COP subjects was similar at TP1 (HRA volume = 4.7±7.6 cm3, COP volume =5.1±7.2 cm3, p= 0.74). The mean synovial volume in HRA subjects increased significantly from TP1 to TP4 (mean volume difference =15.0 cm3, p=0.008) while the COP subjects displayed a minimal increase in mean synovial volume from TP1 to TP4 (mean volume difference =1.1 cm3, p=0.82) (Figure 1). The mean synovial volume in HRA subjects tended to be larger than COP subjects at TP4 and with greater variability (HRA volume= 24.5±76.7 cm3; COP volume= 6.4 ±12.0 cm3, p=0.151). At TP4, 12 cases of ALTRs developed in the HRA subjects (mean time to ALTR = 1.5 yr) compared to 2 cases in the COP subjects (mean time to ALTR = 2.0 yr), p= 0.002 (Figure 2). The risk of ALTRs in HRA subjects was 9.2 (95% CI: 1.60-52.77, p = 0.013) times the risk in COP subjects. The HOOS scores of HRA subjects were similar to COP subjects at all time points for subcategories of Pain and Activities of Daily Living, while HRA subjects had reduced Symptoms at TP1. HRA subjects had better Sporting ability than COP subjects at all time points.Discussion
Previous studies that utilized MRI to evaluate MOM HRAs have focused on imaging findings in patients investigated for painful hip arthroplasty and have been predominantly cross-sectional by design.8,9 This prospective, longitudinal study found a significant increase of synovial volume and higher rate of ALTRs in the HRA subjects, whilst the patient self-assessed symptomatology in the form of HOOS remained slightly better in the HRA subjects than the COP subjects. This suggests that MRI detected ALTRs are not necessarily associated with symptoms. A standardized annual clinical review dependent upon symptomatology alone may miss patients with soft tissue complications until extensive soft tissue damage has occurred. MRI is a non-invasive imaging modality that is uniquely capable of assessing peri-prosthetic soft tissue complications and should be considered as part of the routine follow up for this patient population to allow early detection and monitoring of ALTRs.Acknowledgements
Research reported in this publication was supported by NIH/NIAMS R01AR064840. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.References
1. Laaksonen I, Donahue GS, Madanat R, et al. Outcomes of the Recalled Articular Surface Replacement Metal-on-Metal Hip Implant System: A Systematic Review. J Arthroplasty. 2017;32(1):341-6.
2. Nawabi DH, Hayter CL, Su EP, et al. Magnetic resonance imaging findings in symptomatic versus asymptomatic subjects following metal-on-metal hip resurfacing arthroplasty. The Journal of bone and joint surgery American volume. 2013;95(10):895-902.
3. Sershon R, Balkissoon R, Valle CJ. Current indications for hip resurfacing arthroplasty in 2016. Curr Rev Musculoskelet Med. 2016;9(1):84-92.
4. Koch KM, Lorbiecki JE, Hinks RS, et al. A multispectral three-dimensional acquisition technique for imaging near metal implants. Magnetic resonance in medicine. 2009;61(2):381-90.
5. Potter HG, Nestor BJ, Sofka CM, et al. Magnetic resonance imaging after total hip arthroplasty: evaluation of periprosthetic soft tissue. The Journal of bone and joint surgery American volume. 2004;86-a(9):1947-54.
6. Nawabi DH, Gold S, Lyman S, et al. MRI predicts ALVAL and tissue damage in metal-on-metal hip arthroplasty. Clinical orthopaedics and related research. 2014;472(2):471-81.
7. Nilsdotter AK, Lohmander LS, Klassbo M, et al. Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC musculoskeletal disorders. 2003;4:10.
8. Pandit H, Glyn-Jones S, McLardy-Smith P, et al. Pseudotumours associated with metal-on-metal hip resurfacings. The Journal of bone and joint surgery British volume. 2008;90(7):847-51.
9. Toms AP, Nolan J, Barker T, et al. Early failure of a Birmingham resurfacing hip replacement with lymphoreticular spread of metal debris: pre-operative diagnosis with MR. The British journal of radiology. 2009;82(977):e87-91.
Figures