1395
Simultaneous magnetic resonance elastography of the supraspinatus and the trapezius muscles1Department of Radiological Sciences, Graduate School of Human Health Sciences, Tokyo Metropolitan University, Tokyo, Japan, 2Office of Radiation Technology, Keio University Hospital, Tokyo, Japan, 3Health Research Institute, National Institute of Advanced Industrial Science and Technology, Tsukuba, Japan, 4Department of Judo Neurophysiotherapy, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama, Toyama, Japan, 5Department of Mechanical Engineering, Tokyo Denki University, Tokyo, Japan, 6Department of System Emotional Science, Graduate School of Medicine and Pharmaceutical Sciences, University of Toyama, Toyama, Japan
Synopsis
Palpation is difficult to distinguish stiffness of the supraspinatus and trapezius muscles. Magnetic resonance elastography (MRE) can measure stiffness of tissues quantitatively only if vibrations reach the tissues. We developed simultaneous MRE of the supraspinatus and trapezius muscles by adjusting the shape of a wave transducer and vibration frequency. MREs were performed using self-made wave transducer at 50-150 Hz, with a 25 Hz step. Both wave images of the supraspinatus and trapezius muscles showed clear wave propagation at 50 and 75 Hz. The results demonstrated that our techniques allow simultaneous MRE of the supraspinatus and trapezius muscles at 75 Hz.
INTRODUCTION
Rotator cuff abnormalities are often observed due to aging and overuse and usually occur first at the supraspinatus muscle.1 Mechanical properties such as stiffness of skeletal muscles are altered in various pathophysiologic states.2-4 Therefore, quantitative assessment of stiffness of the supraspinatus muscle should be useful for prevention and evaluation of therapeutic effects of rotator cuff injuries.
Tissue stiffness has been examined clinically using palpation; however, manual palpation is highly subjective and can only examine superficial muscles. Since the supraspinous muscle is located under the trapezius muscle, it is difficult to examine stiffness of the muscle by palpation. Magnetic resonance elastography (MRE) is a noninvasive phase-contrast MR technique that uses mechanical vibration to induce shear waves into a tissue.5 MRE can quantitatively measure stiffness of both superficial and deep tissues. We hypothesized that MRE would allow to differentiate stiffness of the supraspinatus and trapezius muscles.
The purpose of this study was to develop an MRE technique to be applied to the supraspinatus and trapezius muscles simultaneously. We have previously demonstrated that MRE can be applied to the supraspinatus muscle and found the best excitation location.6,7 Hence, this study developed techniques for simultaneous MRE of the supraspinatus and trapezius muscles by adjusting the shape of a wave transducer and vibration frequency.
METHODS
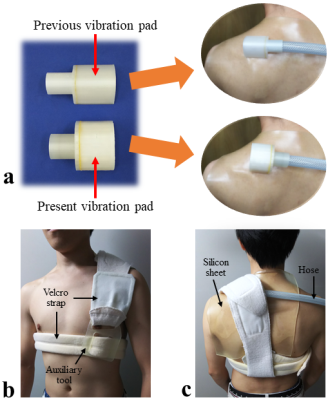
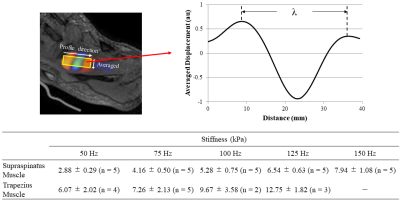
All experiments were performed on a clinical MR imager (Achieva 3.0T; Philips Healthcare, Best, The Netherlands) using a surface coil with subjects in the supine position. In this study, 5 healthy volunteers underwent MRE. A pneumatic vibration was supplied to a wave transducer (vibration pad) that was designed using a three-dimensional (3D) printer (3Dtouch; 3D System, SC, USA) (Fig. 1a). The vibration pad was placed on the skin 2 cm inside and 2 cm above the deltoid tubercle (Fig. 1b,c). MRE acquisitions were performed with a multi-slice gradient-echo type multi-echo MR sequence, and two oblique axial images of the supraspinatus and the trapezius muscles were obtained. In this sequence, readout gradient achieved a similar function to motion-encoding gradient (MEG).8 Vibration frequencies were set at 50-150 Hz, with a 25 Hz step, and they were synchronized with readout gradient. Other acquisition parameters were as follows: 128×128 acquisition matrix, 2 number of averages, 20° flip angle, 180 mm2 field of view, 2 mm slice thickness, AP readout direction (MEG-like direction), 3 ms 1st TE, 40 ms repetition time, and 40 s total acquisition time (4 phase offsets). Stiffness was calculated using the following equation μ = ρ (f. λ)2, where ρ was the muscle density (≒ 1 g/cm3), f was the frequency and λ is the wavelength.RESULTS
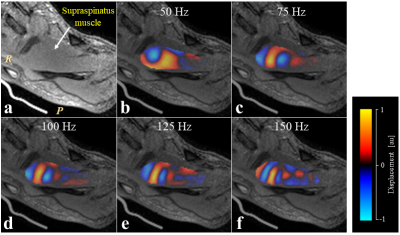
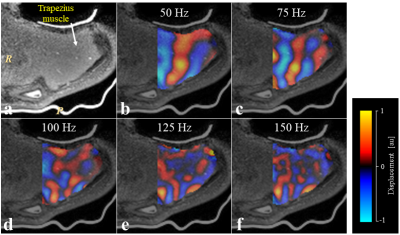
In the supraspinatus muscle, the wave images for all volunteers showed clear wave propagation at all frequencies (Fig. 2). In the trapezius muscle, the wave images for most volunteers showed clear wave propagation at low frequencies (50 and 75 Hz), but those showed unclear wave propagation at high frequencies (100-150 Hz) (Fig. 3). The mean stiffness in the trapezius muscle were larger and larger standard deviation than those in the supraspinatus (Fig. 4).DISCUSSION
Our results indicated that the wave images of both the supraspinatus and trapezius muscles were clear at 50 and 75 Hz. Since a higher frequency provides a higher resolution of stiffness, optimal frequency might be 75 Hz in simultaneous MRE of the supraspinatus and trapezius muscles.
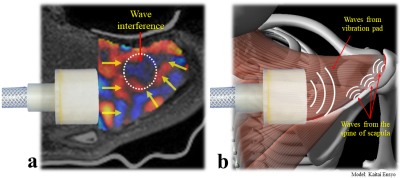
Anatomical locations of these muscles suggest that waves would propagate more easily in the trapezius muscle that is located on the surface than in the supraspinatus muscle. However, the resultant wave images of the trapezius muscle were unclear at high frequencies although those of the supraspinatus muscle were clear. There might be 2 reasons for this discrepancy. The first is the anatomical structure; the trapezius muscle is thinner and more curved than the supraspinatus muscle. These differences of the structures might affect wave propagation. The second is waves from the spine of the scapula. Some wave images at high frequency showed waves propagating from the distal to proximal sides of the trapezius muscle (Fig. 5). We assumed that these waves propagated from the spine of the scapula, and that wave interference due to these waves might lead to unclear wave images in the trapezius muscle.
It is noted that the trapezius muscle is major causes of neck pains affecting 45-54% of the general population.9,10 Therefore, stiffness of the trapezius muscle may vary largely even in healthy volunteers.
CONCLUSIONS
We demonstrated that our MRE techniques can simultaneously assess stiffness of the supraspinatus and trapezius muscles at 75 Hz.Acknowledgements
No acknowledgement found.References
1. Matsuki K, Watanabe A, Ochiai S, et al. Quantitative evaluation of fatty degeneration of the supraspinatus and infraspinatus muscles using T2 mapping. J Shoulder Elbow Surg 2014;23(5):636-641.
2. Bensamoun SF, Ringleb SI, Littrell L, et al. Determination of thigh muscle stiffness using magnetic resonance elastography. J Magn Reson Imaging 2006;23(2):242-247.
3. Basford JR, Jenkyn TR, An KN, et al. Evaluation of healthy and diseased muscle with magnetic resonance elastography. Arch Phys Med Rehabil 2002;83(11):1530-1536.
4. Chen Q, Basford J, An KN. Ability of magnetic resonance elastography to assess taut bands. Clin Biomech 2008;23(5):623-629.
5. Muthupillai R, Lomas DJ, Rossman PJ, et al. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science 1995;269(5232):1854-1857.
6. Ito D, Numano T, Mizuhara K, et al. A new technique for MR elastography of the supraspinatus muscle: a gradient-echo type multi-echo sequence. Magn Reson Imaging 2016;34(8):1181-1188.
7. Ito D, Numano T, Mizuhara K, et al. Optimal Excitation Location for Magnetic Resonance Elastography of the Supraspinatus Muscle. In Proceedings of the 25th Annual Meeting of ISMRM, Honolulu, Hawaii, USA, 2017. Abstract 1584.
8. Numano T, Mizuhara K, Hata J, et al. A simple method for MR elastography: a gradient-echo type multi-echo sequence. Magn Reson Imaging 2015;33(1):31-37.
9. Côté P, Jull G, Sutton S. The Saskatchewan Health and Back Pain Survey. The prevalence of neck pain and related disability in Saskatchewan adults. Spine 1998;23(15):1689-1698.
10. Muñoz-Muñoz S1, Muñoz-García MT, Alburquerque-Sendín F, et al. Myofascial trigger points, pain, disability, and sleep quality in individuals with mechanical neck pain. J Manipulative Physiol Ther. 2012;35(8):608-613.
Figures