1392
Quantitative DCE-MRI perfusion imaging of the subchondral bone in knee osteoarthritis1Radiology & Nuclear Medicine, Erasmus MC, Rotterdam, Netherlands, 2Medical Informatics, Erasmus MC, Rotterdam, Netherlands
Synopsis
Changes in subchondral bone in knee osteoarthritis could be a marker of altered fluid dynamics. Perfusion can be visualized and quantified with MRI using dynamic contrast enhanced MRI (DCE-MRI). Using quantitative analysis of DCE-MRI, we compared perfusion in the affected compartment with the non-affected compartment in patients with unicompartmental knee osteoarthritis. We also evaluated the perfusion in subchondral bone marrow lesions (BMLs). Perfusion of the subchondral bone measured with DCE-MRI is not significantly different between the affected and non-affected compartment. Subchondral BMLs are significantly associated with increased perfusion parameters compared to subchondral bone regions without BMLs.
Introduction
Osteoarthritis (OA) is the most frequent form of arthritis and has major consequences for the individual patient and for public health.1 OA of the knee is characterized by degeneration of articular cartilage, synovial inflammation, and changes in the subchondral bone.2 Changes in subchondral bone could be a marker of altered fluid dynamics, which are thought to affect cytokine excretion for regulation and amplification of bone remodeling and cartilage degeneration.3 T2-weighted magnetic resonance imaging (MRI) can be used to depict fluid-containing structures and abnormalities in the knee, including subchondral bone marrow lesions (BMLs). Perfusion can be visualized and quantified with gadolinium-based dynamic contrast enhanced MRI (DCE-MRI). The aims of this study were to 1) evaluate perfusion in subchondral bone of the affected compartment compared to the non-affected compartment within the same knee of patients with unicompartmental knee OA 2) quantitatively analyze perfusion in subchondral BMLs with DCE-MRI.Methods
23 patients with unicompartmental knee OA were prospectively included. Multisequence MRI including DCE-MRI was performed at 3T (GE Discovery MR750) using an 8-channel knee coil. DCE-MRI was acquired using a sagittal fat suppressed 3D SPGR sequence with 35 phases of 10 seconds. Other scan parameters were: field of view 38x38cm, in-plane resolution 1.5x3.0 mm and slice thickness 5 mm. An intravenous contrast agent (0.2 mmol/kg Magnevist (Bayer)) at 2 ml/s starting after the first phase was administered.
To compare the perfusion in the affected compartment with the non-affected compartment, quantitative analysis of DCE-MRI was performed using Ktrans as the main outcome. Ktrans is a measure of capillary permeability. We also measured the flux rate constant Kep. Subchondral bone ROIs were delineated on three slices of both the affected and non-affected compartment. Subsequently, the mean Ktrans and Kep were calculated for each compartment, and compared between the affected and non-affected compartment. Statistical analysis was performed using a paired student’s t-test.
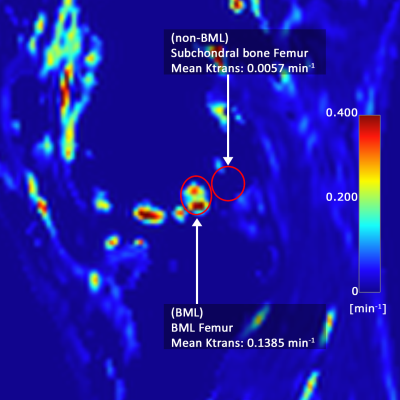
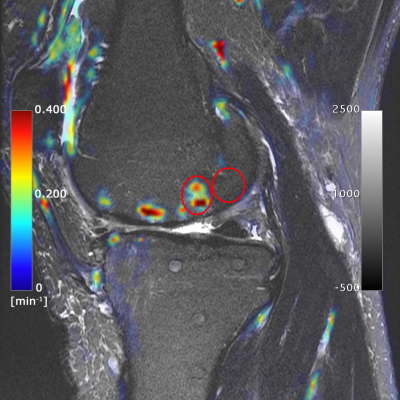
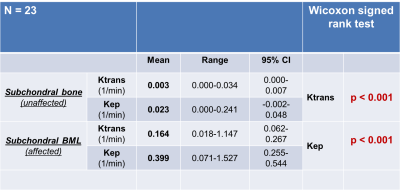
For the evaluation of the perfusion in the subchondral BMLs, regions-of-interest (ROIs) were defined in tibial or femoral subchondral bone containing BMLs and in surrounding subchondral bone without BMLs. These ROIs were defined on fat-saturated T2-weighted images (Figure 1). Again, Ktrans and Kep, were calculated in each ROI (Figure 2 and Figure 3). Mean values were mapped and compared between subchondral bone with and without BMLs using the Wilcoxon signed rank test.
Results
No significant differences were observed between the mean Ktrans and Kep values of the affected and the non-affected compartment in the knee in both the tibia and the femur (P-values 0.137 and 0.773 respectively). Subchondral BMLs detected on fat-saturated T2-weighted images were present in all 23 patients. Perfusion maps and analysis of Ktrans and Kep consistently showed significantly (p<0.001) higher values within subchondral BML ROIs compared to surrounding subchondral bone without BMLs (Figure 4).Conclusion
Perfusion of the subchondral bone measured with DCE-MRI is not significantly different between the affected and non-affected compartment in patients with unicompartmental knee OA. Subchondral BMLs are associated with increased perfusion parameters compared to subchondral bone regions without BMLs. This finding may aid in the understanding of OA pathogenesis and further research is needed to elucidate temporal relationships and correlation with symptoms.Acknowledgements
No acknowledgement found.References
1. Dillon CF, Rasch EK, Gu Q, Hirsch R. Prevalence of knee osteoarthritis in the United States: Arthritis data from the Third National Health and Nutrition Examination Survey 1991-94. J Rheumatol 2006;33:2271-2279
2. F. Berenbaum, Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!), Osteoarthritis and Cartilage, 2013;21(1):16-21.
3. Lee, Jonathan H. et al. “Assessment of Bone Perfusion with Contrast-Enhanced Magnetic Resonance Imaging: Imaging of Bone Marrow Edema Associated with Osteoarthritis and Avascular Necrosis.” The Orthopedic clinics of North America (2009);40(2):249–257.
Figures