1369
Ability of MRI to Predict the Severity and Location of Chondral and Labral Pathology at Arthroscopy1Hospital for Special Surgery, New York, NY, United States
Synopsis
Preoperative MRI and intraoperative arthroscopic images were independently reviewed in a cohort of 24 hips with femoroacetabular impingement with respect to severity and location of chondral, labral, and osseous pathology. Initial calculation of agreement between MRI and arthroscopic findings demonstrated fair to near perfect agreement for the severity of pathology; however, agreement for the location of pathology was highly variable. MR images were subsequently re-scored utilizing the indirect head of the rectus femoris as an anatomic landmark, in accordance with the system used by the operating surgeon, resulting in overall increased agreement across position-dependent variables.
Introduction
Femoroacetabular impingement (FAI) has been recognized as a common cause of early labral and chondral damage. Hip preservation surgery has been shown to relieve pain with correction of the underlying osseous deformity and labral pathology, particularly in individuals who lack significant chondral damage at the time of intervention1. Magnetic resonance imaging (MRI) provides an effective, non-invasive means of detecting chondral and labral pathology in patients with FAI, given its ability to generate high resolution images with excellent soft tissue contrast2,3,4. While the ability of MRI to detect such pathology has been established, the degree to which MRI findings correlate with findings observed at surgery remains unclear. The purpose of this study was to investigate the ability of MRI to predict the severity and location of arthroscopically detected soft tissue lesions in patients with FAI.Methods
Twenty-four hips in 21 patients (26±6 years) undergoing hip arthroscopy for FAI were retrospectively reviewed. Pre-operative multi-planar morphologic MRI was assessed by a fellowship trained musculoskeletal radiologist. Blinded intraoperative videos were reviewed by an experienced fellowship trained operating surgeon. Arthroscopic and MR images were evaluated for presence of ligamentum teres tear, anterior inferior iliac spine (AIIS) morphology, acetabular and femoral cartilage defects (ALAD and Outerbridge score), Beck classification of labral pathology, and location of chondral and labral injury using a clock face methodology. Gwet’s agreement coefficients (AC; range -1.0, 1.0) were calculated. Following initial evaluation, MR images were subsequently re-scored by two independent readers (both fellowship trained musculoskeletal radiologists) utilizing the indirect head of the rectus femoris as an anatomic landmark to demarcate 12:00 on the clock-face (Figure 1), in accordance with the methodology followed by the operating surgeon, to assess agreement between readers as well as between MRI and arthroscopy.Results
Initial evaluation demonstrated substantial (AC=0.687-0.723) agreement between MRI and arthroscopy for ligamentum teres tear, AIIS Type, and Beck classification. There was moderate to near perfect (0.458-0.957) agreement for transitional zone delamination, fair to near perfect (0.378-0.957) agreement for acetabular chondral defects, moderate to near perfect (0.538-0.957) agreement for femoral chondral defects. Agreement for labral tears using a clock-face assessment of location was highly variable (-0.821-0.957). Subsequent reevaluation of MR images utilizing the indirect head of the rectus femoris as an anatomic landmark demonstrated overall improved agreement with arthroscopic findings at nearly all locations for position-dependent variables (24/27, 88.9%) with respect to both chondral and labral pathology (Figure 2). Agreement coefficients between MRI readers were substantial to near perfect, except for several zones in which AC was incalculable due to perfect raw agreement between readers (Figure 2).Discussion
Fair to near perfect agreement was found between MRI and arthroscopic evaluation of chondral and labral damage upon initial evaluation; however, agreement tended to be reduced in specific anatomic areas. Utilization of the indirect head of the rectus femoris as an anatomic landmark to establish the 12:00 position on both MRI and arthroscopy resulted in overall improved agreement for localization of soft tissue pathology, and proved reliable between MRI readers.Conclusion
MRI provides a noninvasive means of accurately detecting and localizing chondral and labral pathology in patients with femoroacetabular impingement, with improved agreement between imaging and surgical findings when a consistent anatomic landmark is utilized as a reference for describing location of pathology.Acknowledgements
Research reported in this publication was supported by NIH/NIAMS R01AR066069. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
HSS has an institutional research agreement in place with GE Healthcare
References
1. Bedi A, Kelly BT. Femoroacetabular Impingement. JBJS Am 2013, 95(1):82-92.
2. Li AE, Jawetz ST, Greditzer HG, Burge AJ, Potter HG. MRI for the preoperative evaluation of femoroacetabular impingement. Insights in Imaging 2016, 7(2): 187-98.
3. Li AE, Jawetz ST, Greditzer HG, Burge AJ, Nawabi DH, Potter HG. MRI Evaluation of Femoroacetabular Impingement After Hip Preservation Surgery. AJR 2016, 207(2): 392-400.
4. Gold SL, Burge AJ, Potter HG. MRI of Hip Cartilage: joint morphology, structure, and composition. CORR 2012, 4(6): 518-34.
Figures
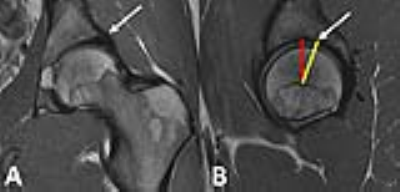
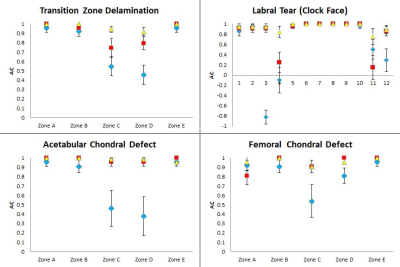
Figure 2:
Gwet’s agreement coefficients (AC, mean± SE) for MRI versus arthroscopic
localization of chondral and labral pathology with (red square) and without
(blue diamond) utilization of the rectus femoris indirect head as an anatomic
landmark. AC between MRI readers (yellow triangle) was substantial to almost
perfect for all variables.
Note: Values at the “1” level represent raw agreement, as AC is incalculable in the setting of perfect agreement.