1268
Tongue deformation during mandibular advancement, as determined using tagged-MRI, may help to predict mandibular advancement treatment outcome in Obstructive sleep apnoea.1Neuroscience Research Australia, Sydney, Australia, 2School of Medical Sciences, University of New South Wales, Sydney, Australia, 3Prince of Wales Hospital, Sydney, Australia, 4Department of Respiratory and Sleep Medicine, Royal North Shore Hospital, Sydney, Australia, 5Charles Perkins Centre, University of Sydney, Sydney, Australia, 6Prince of Wales Clinical School, University of New South Wales, Sydney, Australia
Synopsis
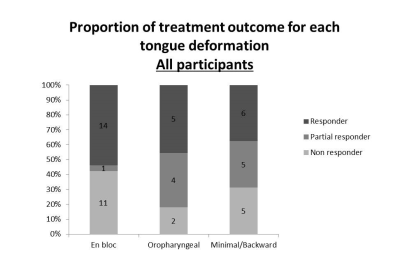
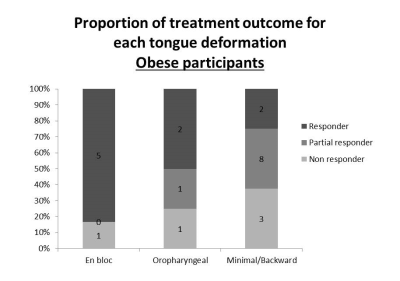
Tongue deformation during mandibular advancement, as characterised by tagged-MRI, may be helpful to predict mandibular advancement splint (MAS) therapy for obstructive sleep apnea (OSA). 68 OSA patients untreated underwent a MRI scan prior to trialling a MAS and treatment outcome was determined. Preliminary results identified 3 possible tongue deformations (en bloc, oropharyngeal and minimal/backward) with variable impact on the upper airway size. Over all participants, tongue deformation was not associated with treatment outcome, but among obese participants, “en bloc” tongue deformation was associated with positive treatment outcomes. This may also improve the understanding of the mechanisms underpinning MAS therapy effectiveness.
Introduction
At least 5% of adults have obstructive sleep apnoea (OSA)1, a respiratory disorder associated with a high risk of accidents and increased risk of cardiovascular disease2. OSA can be treated by wearing a mandibular advancement splint (MAS) to hold the mandible in a forward position3 during sleep. However, the efficacy of the treatment is variable between patients, and there are currently no reliable methods to predict treatment outcomes4.
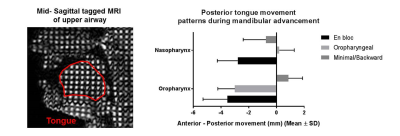
Using tagged magnetic resonance imaging (MRI), we have previously observed 3 different tongue deformation patterns during mandibular advancement in OSA patients5. 1- “En bloc”, which enlarged the airway by moving forward the posterior section of the tongue via a shortening of the tissue; 2- “Oropharyngeal”, which only enlarged the lower part of the airway; 3- “Minimal”, which was associated with an elongation of the tongue without enlargement of the pharyngeal airway. In the current study, aim to develop an MRI biomarker for MAS treatment outcome based on tongue deformation, informed by previous studies that show airway enlargement contributes to positive treatment outcomes6.
Methods
68 untreated OSA participants (18 women, aged 19-72 years, Body mass index - BMI 17-51 kg/m2) underwent a MRI scan (Achieva 3TX, Philips) prior to clinically trialling a MAS. The severity of OSA is measured by the apnoea hypopnoea index (AHI), which is the number of apnoeas and hypopnoeas per hour of sleep. 20 subjects had Mild OSA (5<AHI≤15 events/h), 27 moderate OSA (15<AHI≤30 events/h) and 21 had severe OSA (AHI>30 events/h). Tagged MRI images were collected by superimposing a grid on the tissues using a spatial modulation of magnetization sequence, and then 8 images were acquired every 250 ms during mandibular advancement5. Tongue deformation was quantified using harmonic phase methods7. Imaging parameters: TR/TE = 400/16 ms, FOV = 220x196 mm, slice thickness = 10 mm, in-plane spatial resolution = 0.86x0.86 mm2, tag spacing = 8.6 mm. Treatment outcome was determined by comparing polysomnography results at enrolment to a repeat study 12 weeks after the start of the therapy.Results
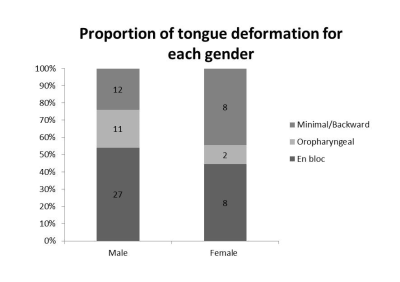
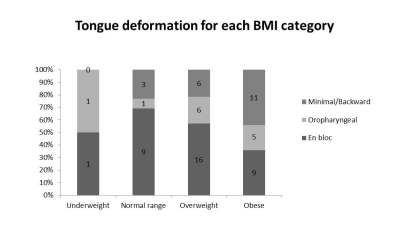
During mandibular advancement, 35 OSA participants showed an “en bloc” deformation, 13 “oropharyngeal”, 20 “minimal/backward” (Figure 1). A larger proportion of men had an “en bloc” deformation (54%) (Figure 2). An increase in BMI was associated with a decrease in the anterior movement of the oropharyngeal and nasopharyngeal posterior tongue (Spearman, P = 0.04 for both) (Figure 3). No relationship was seen between age and the anterior movement of the tongue in either oropharyngeal or nasopharyngeal regions (Spearman, P = 0.42, P = 0.77, respectively). Over all participants, tongue deformation was not associated with treatment outcome (Figure 4), but among obese participants, “en bloc” tongue deformation was associated with positive treatment outcomes (Figure 5).Conclusion
Preliminary results showed the presence of several distinct tongue deformation patterns during mandibular advancement, which may be a useful biomarker of treatment outcomes. The results may also improve our understanding of the mechanisms underpinning MAS therapy effectiveness.Acknowledgements
This study was funded by the National Health and Medical Research Council of Australia.References
1. Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136-143.
2. Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease. J Am Coll Cardiol. 2008;52(8):686-717.
3. Bamagoos AA, Sutherland K, Cistulli PA. Mandibular Advancement Splints. Sleep Med Clin. 2016;11(3):343-352.
4. Mehta A, Qian J, Petocz P, Darendeliler MA, Cistulli PA. A randomized, controlled study of a mandibular advancement splint for obstructive sleep apnea. Am J Respir Crit Care Med. 2001;163(6):1457-1461.
5. Brown EC, Cheng S, McKenzie DK, Butler JE, Gandevia SC, Bilston LE. Tongue and lateral upper airway movement with mandibular advancement. Sleep. 2013;36(3):397-404.
6. Chan AS, Sutherland K, Schwab RJ, et al. The effect of mandibular advancement on upper airway structure in obstructive sleep apnoea. Thorax. 2010;65(8):726-732.
7. Osman NF, Kerwin WS, McVeigh ER, Prince JL. Cardiac motion tracking using CINE harmonic phase (HARP) magnetic resonance imaging. Magn Reson Med. 1999;42(6):1048-1060.
Figures