1257
Comparison of Staging Capability among PET/MRI, MRI, PET/CT and Conventional Staging Method in Patients with Malignant Pleural Mesothelioma1Division of Functional and Diagnostic Imaging Research, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 2Advanced Biomedical Imaging Research Center, Kobe University Graduate School of Medicine, Kobe, Japan, 3Toshiba Medical Systems Corporation, Otawara, Japan, 4Division of Radiology, Department of Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 5Center for Radiology and Radiation Oncology, Kobe University Hospital, Kobe, Japan
Synopsis
No direct comparisons for TNM staging capability among whole-body PET/CT, whole-body PET/ MRI, whole-body MRI and conventional radiological examination in malignant pleural mesothelioma (MPM). We hypothesize that whole-body FDG-PET/MRI and MRI have better potential for TNM stage assessment than whole-body FDG-PET/CT and conventional staging method in MPM patients. The purpose of this study was to directly and prospectively compare the TNM staging capability among whole-body FDG-PET/MRI, MRI with DWI, FDG-PET/CT and conventional staging method in MPM patients
Introduction
Malignant pleural mesothelioma (MPM) has a very poor prognosis; the median survival after diagnosis ranges between 4 and 18 months. Imaging plays an important role in the diagnosis and staging of MPM, because biopsy and video-assisted thoracoscopic surgery carry the risk of tumor seeding and should therefore be avoided if possible. A large group of noninvasive imaging modalities such as ultrasound (US), computed tomography (CT), and positron emission tomography (PET) or PET combined with CT (PET/CT) using 2-[fluorine-18]-fluoro-2-deoxy-D-glucose (FDG), magnetic resonance imaging (MRI) is currently used, but the diagnosis of MPM remains challenging. CT is widely used as the primary imaging modality for clinical evaluation and diagnosis of MPM. In the last decades, integrated FDG-PET/CT has been suggested as the standard technique for the staging of MPM, because it combines metabolic and anatomic information. Moreover, whole-body MR imaging has been suggested as useful for lung cancer staging in the last decade (1, 2), and PET combined with MR imaging (PET/MRI) is now suggested as useful and tested for oncologic patients including lung cancer (3). However, no direct comparisons for TNM staging capability among whole-body PET/CT, whole-body PET/ MRI, whole-body MRI and conventional radiological examination in MPM. We hypothesize that whole-body FDG-PET/MRI and MRI have better potential for TNM stage assessment than whole-body FDG-PET/CT and conventional staging method in MPM patients. The purpose of this study was to directly and prospectively compare the TNM staging capability among whole-body FDG-PET/MRI, MRI with DWI, FDG-PET/CT and conventional staging method in patients with MPM.Materials and Methods
Twenty-three consecutive and pathologically diagnosed MPM patients (15 men, 8 women; mean age 60 years) prospectively underwent whole-body MRI, integrated PET/CTs, conventional staging method, surgical resection, pathological examination, and more than 2-year follow-up examinations. All whole-body MRI including DWI were obtained by using a 3T MR system (Vantage Titan 3T, Toshiba Medical Systems) with multi-channel body and spine coils as having parallel imaging capability (Atlas SPEEDER, Toshiba Medical Systems). All co-registered MR/PETs were generated by means of our proprietary software. The final TNM staging in each patient was determined based on tumor board reviewing all examination results. Then, T, N and M factors as well as tumor stage in each patient were prospectively assessed by all methods. To evaluate agreements of all factors and stage between each method based on consensus reading and final diagnosis, kappa statistics were also performed. Diagnostic accuracy of each factor and clinical stage were also statistically compared each other by using McNemar’s test. Agreements were considered as poor for κ< 0.21, fair for κ = 0.21–0.40, moderate for κ = 0.41–0.60, substantial for κ = 0.61–0.80, and excellent for κ = 0.81–1.00. A p value < 0.05 was considered statistically significant for all statistical analyses.Results
Representative case is shown in Figure 1 and 2. Agreements for T and N factors on whole-body PET/MRI and MRI with DWI (0.86≤κ≤1.00, p<0.0001), and substantial PET/CT and conventional staging method (0.61≤κ≤0.73, p<0.0001). In addition, agreements of whole-body PET/MRI, MRI with DWI and PET/CT were almost perfect (κ=1.00, p<0.0001), and moderate on conventional staging method (κ=0.47, p<0.0001). Moreover, agreements for TNM staging were determined as almost perfect on whole-body PET/MRI and MRI with DWI (κ=0.87, p<0.0001), and substantial on PET/CT and conventional staging method (κ=0.70, p<0.0001). Accuracies of all factors and TNM staging are shown in Figure 3. On N factor assessment, accuracy of whole-body PET/MRI (100 [23/23] %) and MRI with DWI (100 [23/23] %) were significantly higher than that of conventional staging method (73.9 [17/23] %, p=0.04).Conclusion
Whole-body PET/MRI and MRI with DWI have better potential for TNM staging than conventional staging method, and are considered at least as valuable as PET/CT in patients with malignant pleural mesothelioma.Acknowledgements
This study was supported by Toshiba Medical Systems and Bayer Pharma.References
- Ohno Y, Koyama H, Onishi Y, et al. Radiology. 2008; 248(2): 643-654.
- Takenaka D, Ohno Y, Matsumoto K, et al. J Magn Reson Imaging. 2009; 30: 298-308.
- Ohno Y, Koyama H, Yoshikawa T, et al. Radiology. 2015; 275: 849-861.
Figures

Figure 1. 72-year-old female patient with malignant mesothelioma (pT4N0M0: pStage IV) due to diffuse extension of tumor into chest wall (arrow).
(L to R: Thin-section MPR image, PET/CT, STIR image, DWI and PET/MRI): STIR image and PET/MRI clearly demonstrate chest wall invasion of MPM, although thin-section MPR image, PET/CT and DWI are not diagnosed as having chest wall invasion of MPM. This patient was assessed as clinical stage as stage IV (T4N0M0) on whole-body PET/MRI and MRI with DWI, and stage II (T2N0M0) on PET/CT and conventional staging method.

Figure 2. 68-year-old male patient with malignant methothelioma (pT2N3M0: pStage IV) due to direct diaphragm muscle invasion and bilateral mediastinal lymph node metastases (arrow and arrow head).
(L to R: Thin-section MPR image, PET/CT, STIR image, DWI and PET/MRI): STIR image, DWI and PET/MRI clearly demonstrate contralateral lymph node metastases of MPM, and diagnosed asN3, although thin-section MPRimage and PET/CT were diagnosed as N0 and N2 in this case. This patient was assessed as clinical stage as stage IV (T2N3M0) on whole-body PET/MRI and MRI with DWI, and stage II (T2N0M0) on conventional staging method and stage III (T2N2M0) on PET/CT .
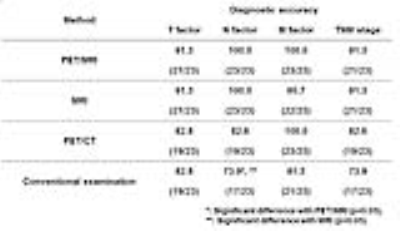
Figure 3. Comparisons of accuracy of each factor and stage among all methods.
On N factor assessment, accuracy of whole-body PET/MRI and MRI with DWI were significantly higher than that of conventional staging method (p=0.04).