1243
Anatomical variation of age-related changes in vertebral bone marrow composition using chemical shift encoding-based water-fat MRI1Department of Neuroradiology, Technical University of Munich, Munich, Germany, 2Department of Radiology, Technical University of Munich, Munich, Germany, 3Department of Nutritional Medicine, Technical University of Munich, Munich, Germany
Synopsis
The assessment of vertebral bone marrow water-fat composition is attracting growing interest for applications in osteoporosis and bone metabolism. Chemical shift encoding-based water-fat MRI allows spatially resolved assessment of proton density fat fraction (PDFF) at the spine. This study demonstrated that males started with greater PDFF values in the Twenties compared to females. However, females showed an accelerated bone marrow fatty conversion until the Seventies on. This finding can be explained by the (patho-)physiological process of menopause. Interestingly, the relative age-related PDFF changes from the Twenties to the Seventies were dependent on the anatomical location and were most pronounced at lower lumbar vertebral levels in both genders.
Purpose
Assessment of vertebral bone marrow water–fat composition has been proposed as advanced imaging biomarker for osteoporosis associated fracture risk prediction [1,2]. Furthermore, changes of the bone marrow play an important role in disorders of the hematopoietic system and metabolic disorders including obesity and diabetes [3]. However, reference values of the vertebral bone marrow fat fraction with regard to age and gender have been so far primarily obtained by using 1H-MRS [4,5]. Chemical shift encoding-based water-fat MRI allows spatially resolved assessment of bone marrow fat composition [6]. A gender-independent increase of proton density fat fraction (PDFF) with age has been recently reported in children and a decrease of PDFF from the lumbar to the cervical spine has been reported in both young adults and children [7,8]. In children, it has been also shown that anatomical variation of PDFF from the lumbar to the cervical spine is age dependent. Therefore, the purpose of our study was to investigate the anatomical variation of age-related PDFF changes at the lumbar spine in male and female adults by using chemical shift encoding-based water-fat MRI.Methods
Subjects: 156 subjects with no history of pathological bone changes were recruited for this study: age range 20–29 years: 12/30 males/females; 30–39: 15/9 males/females; 40–49: 4/14 males/females; 50–59: 9/27 males/females; 60–69: 5/19 males/females; 70–79: 4/8 males/females (Fig. 1).
MR Imaging: All subjects underwent 3T MRI (Ingenia, Philips Healthcare). An eight-echo 3D spoiled gradient-echo sequence was used for chemical shift-encoding based water-fat separation at the lumbar spine using the built-in-the-table posterior coil elements (12-channel array). The sequence acquired the eight echoes in a single TR using non-flyback (bipolar) read-out gradients and the following imaging parameters: TR/TE1/ΔTE = 11/1.4/1.1 ms, FOV = 220×220x80 mm3, acquisition matrix = 124×121, voxel size = 1.8x1.8x4.0 mm³, receiver bandwidth = 1527 Hz/pixel, frequency direction = A/P (to minimize breathing artifacts), 1 average, scan time = 1min and 17 s. A flip angle of 3° was used to minimize T1-bias effects.
Fat Quantification: The gradient echo imaging data were processed on-line using the fat quantification routine of the vendor. The routine performs first a phase error correction and then a complex-based water–fat decomposition using a pre-calibrated seven-peak fat spectrum and a single T2* to model the signal variation with echo time and compute PDFF maps. Segmentation of the vertebral bodies L1 to L4 were manually performed on the PDFF maps using the free open-source software Medical Imaging Interaction Toolkit (Fig. 2). According to DXA measurements, PDFF values were extracted at each vertebral level from L1 to L4.
Results
Mean PDFF averaged over L1-4 was significantly (p<0.05) higher in males than females in the Twenties (32.0±8.0% vs. 27.2±6.0%) and Thirties (35.3±6.7% vs. 27.3±6.2%). With increasing age females showed an accelerated fatty conversion of the bone marrow compared to men with no significant (p>0.05) mean PDFF differences in the Forties (males: 32.4±8.4%; females: 34.5±6.8%) and Fifties (males: 42.0±6.1%; women: 40.5±9.7%). The accelerated conversion process continued resulting in greater mean PDFF values in females than males in the Sixties (males: 40.2±6.9%; females: 48.8±7.7%; p=0.033) and Seventies (males: 43.9±7.6%; females: 50.5±8.2%; p=0.208) (Fig. 3). PDFF increased from L1 to L4 in all subjects (L1: 35.9±11.7%; L2: 36.2±10.9%; L3: 37.2±10.7%; L4: 39.5±11.2% with L1-2: p=0.303; L2-3: p<0.001; L3-4: p<0.001)). Relative age-related PDFF change from the Twenties to the Seventies increased from L1 to L4 in both genders (Fig. 4 and 5). The relative age-related PDFF change from the Twenties to the Seventies increased from 16.7% (L1) to 51.4% (L4) in males and was mostly constant in females ranging between 76.8% (L1) and 85.7% (L4). The PDFF changes through the five age groups were significantly different at all vertebral levels in females and at L3 and L4 level in males.Discussion & Conclusion
Vertebral PDFF assessed with chemical shift encoding-based–fat MRI was dependent on age and gender in adults. An accelerated fatty conversion of the bone marrow was observed in females with increasing age due to menopause. Relative age-related PDFF changes from the Twenties to the Seventies showed an anatomical variation with most pronounced changes at lower lumbar vertebral levels in both genders. The results allow insights in physiological changes of the vertebral bone marrow composition and may serve as reference data. Given the reported anatomical variation of age-related changes in vertebral bone marrow, the results suggest that a spatially-resolved PDFF map might be preferable to single-voxel MRS-based PDFF measurements.Acknowledgements
The present work was supported by the European Research Council (grant agreement No 677661 – ProFatMRI and grant agreement No 637164 – iBack), TUM Faculty of Medicine KKF grant H01 and Philips Healthcare.References
1. Patsch et al.: Bone marrow fat composition as a novel imaging biomarker in postmenopausal women with prevalent fragility fractures. J Bone Miner Res 2013; 28:1721.
2. Schwartz et al.: Vertebral bone marrow fat associated with lower trabecular BMD and prevalent vertebral fracture in older adults. J Clin Endocrinol Metab. 2013; 98:2294.
3. Cordes et al.: MR-Based Assessment of Bone Marrow Fat in Osteoporosis, Diabetes, and Obesity. Frontiers in Endocrinology. 2016; 7:74.
4. Kugel et al.: Age- and sex-specific differences in the 1H-spectrum of vertebral bone marrow. J Magn Reson Imaging. 2001; 13:263.
5. Griffith et al.: Bone marrow fat content in the elderly: a reversal of sex difference seen in younger subjects. J Magn Reson Imaging. 2012; 36:225.
6. Karampinos et al. Quantitative MRI and spectroscopy of bone marrow. J Magn Reson Imaging. 2017 [Epub ahead of print].
7. Baum et al.: Assessment of whole spine vertebral bone marrow fat using chemical shift-encoding based water-fat MRI. J Magn Reson Imaging. 2015; 42:1018. 8. Ruschke et al.: Measurement of vertebral bone marrow proton density fat fraction in children using quantitative water-fat MRI. MAGMA 2017 [Epub ahead of print].
Figures
Fig. 1:
Mean and Standard Deviation (SD) of age and BMI for each age group. P-values indicate differences between male and female subjects in the respective age group.
Fig. 2:
Representative segmentation of the vertebral bodies of L1 to L4 in the PDFF maps of a 22 (A) and 61(B) year old female, respectively. Note the lower PDFF values in A (mean PDFF: 26.2%) than in B (mean PDFF: 62.1%).
Fig. 3:
Mean PDFF values (averaged over L1-4) of both genders for each age group. Bold p-values indicate statistically significant differences between male and female subjects.
Fig. 4:
Anatomical variation of PDFF values for each age group and gender. Relative age-related PDFF change was computed as: (mean PDFF Seventies – mean PDFF Twenties) / mean PDFF Twenties. Bold p-values indicate significantly (p<0.05) different PDFF values through the five age groups at respective vertebral level.
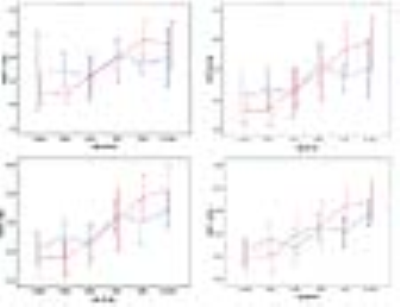
Fig. 5:
Mean and Standard Deviation of PDFF values for males (blue) and females (red) in L1 to L4. Note the pronounced age-related fatty bone marrow conversion at lower lumbar vertebral levels.