1177
Cervical cancer staging and surveillance using Restriction Spectrum Imaging (RSI)-MRI in comparison to PET-CT: Pilot Clinical Application1Radiology, University of California, San Diego, San Diego, CA, United States, 2Radiation Medicine and Applied Sciences, University of California, San Diego, La Jolla, CA, United States, 3Radiology & Neurosciences, University of California, San Diego, La Jolla, CA, United States
Synopsis
This proof of concept study suggests restriction spectrum imaging (RSI)-magnetic resonance imaging (MRI) provides similar cervical cancer staging and surveillance information compared to standard of care MP-MRI and PET-CT. Advantages over the standard of care modalities may include improved cost-effectiveness, brevity, radiation-free, and contrast media-free. Pilot cases suggest that RSI-MRI cellularity index can detect residual and recurrent tumor in post-treatment cervical cancer patients with similar sensitivity to PET-CT. RSI-MRI has the advantage of minimal false positive results related to radiation-related post-treatment changes that often confound interpretation of PET-CT.
Introduction
Contrast enhanced pelvic MRI and PET-CT are standard of care for staging, surveillance and predicting survival outcome in cervical cancer patients.1-2 However, evaluation of residual or recurrent tumor by PET-CT in the first few months after chemotherapy and radiation therapy is typically confounded by post-treatment changes. Patients typically wait 3 months post treatment to evaluate response to treatment for cervical cancer with PET-CT due to false positive sensitivity to post-treatment changes.2 Furthermore, imaging workup with PET-CT results in the use of ionizing radiation and intravenous contrast agents. To overcome these drawbacks, we used an advanced magnetic resonance imaging (MRI) diffusion technique termed restriction spectrum imaging (RSI)-MRI that we hypothesize is not susceptible to false positive post-treatment changes with additional advantages of being a radiation- and contrast media-free exam. RSI-MRI has been useful in oncologic evaluation in both brain and prostate imaging.3-5 This is the first application of evaluating RSI-MRI in cervical cancer.Methods
All patients in this IRB–approved study were previously diagnosed with cervical cancer status by Pap smear or conoscopy. Prior to radiation therapy, a pelvic MRI was performed using a 3.0-T SignaHDxt MRI Scanner (General Electric). Standard pelvic MRI sequences, covering the cervix, uterus and ovaries, included axial and sagittal T2, DWI, and axial T1 plus axial water/fat ASSET or axial FSPGR T1 pre- and post-contrast imaging (with Gadobutrol intravenous contrast). The RSI-MRI protocol parameters included b-values of 0, 125, 375, and 1,000 s/mm2 (6, 6, and 15 unique diffusion directions for all nonzero b-values, respectively). The RSI-MRI protocol is completed in about 5 min. RSI-MRI cellularity maps were reconstructed based on all b-values and standardized across the samples.Results
Sixteen patients, representing a range of cervical tumor aggressiveness, were evaluated by PET-CT, contrast-enhanced MRI, and RSI-MRI, almost all of them prior to treatment/radiation therapy. Detection of cervical cancer by RSI-MRI cellularity index performed as well as SUV derived from FDG-PET (16/16 cases detected by PET-CT were detected by RSI-MRI; RSIave = 6.2 ± 2.1 (based on z-scoremax across all patients); SUVmax = 16.4 ± 7.6). In addition, 2 patients underwent surveillance RSI-MRI and PET-CT before and after treatment. RSI-MRI detected response to treatment equally as PET-CT (2/2 cases).Discussion/Conclusion
This proof of concept study suggests RSI-MRI cellularity provides similar information as PET-CT in terms of staging and surveillance of cervical cancer with the advantage of no radiation and less false positive sensitivity to post-treatment artifacts. Future investigation will focus on determining if RSI-MRI cellularity can detect residual or recurrent tumor following treatment for cervical cancer in a larger patient cohort, with PET-CT as the reference standard.
Acknowledgements
We appreciate funding from the UCSD Clinician Scientist Program (#5T32EB005970-07) (G.Y.), Radiological Society of North America (RSNA) (#AMER RR1604) (K.Z., L.M.), UCSD Academic Senate (#RES GRT RP34H-MELL) (L.M.), and General Electric (R.R., A.M.D.).References
1. Bourgioti C, Chatoupis K, & Moulopoulos LA (2016) Current imaging strategies for the evaluation of uterine cervical cancer. World J Radiol 8(4):342–354.
2. Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW. Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. JAMA 2007;298(19):2289-95.
3. White NS, McDonald C, McDonald CR, Farid N, Kuperman J, Karow D, Schenker-Ahmed NM, Bartsch H, Rakow-Penner R, Holland D, Shabaik A, Bjørnerud A, Hope T, Hattangadi-Gluth J, Liss M, Parsons JK, Chen CC, Raman S, Margolis D, Reiter RE, Marks L, Kesari S, Mundt AJ, Kane CJ, Kaine CJ, Carter BS, Bradley WG, & Dale AM. Diffusion-weighted imaging in cancer: physical foundations and applications of restriction spectrum imaging. Cancer Res 2014; 74(17):4638-4652.
4. White NS, Leergaard TB, D'arceuil H, Bjaalie JG, Dale AM. Probing tissue microstructure with restriction spectrum imaging: histological and theoretical validation. Human brain mapping 2013; 34(2): 327-346.
5. Rakow-Penner RA, White NS, Parsons JK, Choi HW, Liss MA, Kuperman JM, Schenker-Ahmed N, Bartsch H, Mattrey RF, Bradley WG, Shabaik A, Huang J, Margolis DJ, Raman SS, Marks L, Kane CJ, Reiter RE, Karow DS, Dale AM. Novel technique for characterizing prostate cancer utilizing MRI restriction spectrum imaging: proof of principle and initial clinical experience with extraprostatic extension. Prostate Cancer Prostatic Dis 2015; 18(1):81-5.
Figures
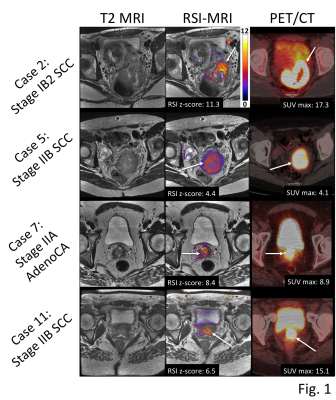
Fig. 1. MRI and PET/CT for four cervical cancer patients. Column 1, T2-weighted MRI; column 2, RSI z-score maps overlaid on T2-weighted MRI; column 3, PET/CT.
Abbreviations: AdenoCA, adenocarcinoma; CT, computed tomography; PET, positron emission tomography; MRI, magnetic resonance imaging; RSI, restriction spectrum imaging; SCC, squamous cell carcinoma; SUVmax, standardized uptake value.
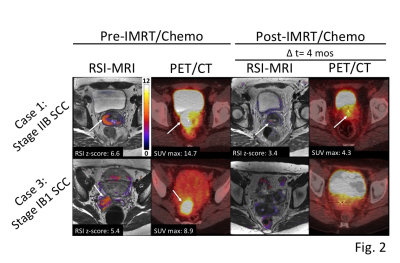
Fig. 2. MRI and PET/CT for two cervical cancer patients pre- and post-IMRT/chemotherapy. Column 1, RSI z-score maps overlaid on T2-weighted MRI (RSI-MRI) pre-IMRT/chemotherapy; column 2, PET/CT pre-IMRT/chemotherapy; column 3, RSI-MRI post-IMRT/chemotherapy (Δt = 4 months); column 4, PET/CT post-IMRT/chemotherapy (Δt = 4 months).
Abbreviations: CT, computed tomography; IMRT, intensity-modulated radiation therapy; PET, positron emission tomography; MRI, magnetic resonance imaging; RSI, restriction spectrum imaging; SCC, squamous cell carcinoma; SUVmax, standardized uptake value.