1085
Comparing 19F C3F8 Lung Ventilation Imaging with Hyperpolarized 129Xe: Similarities and Limitations1POLARIS, Academic Radiology, University of Sheffield, Sheffield, United Kingdom, 2GE Healthcare Inc., Aurora, OH, United States
Synopsis
Fluorinated gases are a cheaper alternative to hyperpolarized gas for lung ventilation imaging. However, lower resolution images are necessitated by the inherently smaller MR signal from 19F. Within this study we determine the feasibility of using C3F8 for lung ventilation imaging by comparing quantitative metrics of lung function obtained from ventilation images of 19F with those obtained from ventilation images of hyperpolarized 129Xe. A reproducibly lowered coefficient of variation distribution was observed due to lower resolution of 19F imaging. However, ventilation images acquired with 19F were of comparable SNR to those using 129Xe.
Background
Lung ventilation imaging of inert gases may be performed with inhaled hyperpolarized (HP) gases (3He or 129Xe), or fluorinated gases (SF6, C2F6, C3F8)1. Quantitative measures of lung function, such as ventilation volume percentage (%VV), and the coefficient of variation of signal intensity (CV)2, have previously been derived from inhaled HP gases lung ventilation imaging. Lung ventilation imaging with inhaled fluorinated gas is a cheaper alternative to HP gas imaging, and does not require specialized polarization equipment1. In addition, fluorinated gases can be mixed with oxygen, allowing greater potential for dynamic imaging of wash-in/wash-out dynamics3. However, the inherently low MR signal and short T2* of fluorinated gases results in lower signal-to-noise ratio (SNR) and necessitates lower image resolution when compared to HP gas imaging. Recently, there have been significant improvements in sequence optimization for fluorinated gas imaging using ultrashort echo time and steady state free precession methods4,5. However, to date, there has been no clear demonstration that fluorinated gas imaging can be used routinely to provide suitably robust quantitative measures of lung function. Additionally, fluorinated gases do not yet have the same established evidence base in clinical applications that 129Xe imaging has6.
Purpose
To compare metrics of lung function derived from images acquired using 129Xe and 19F imaging in healthy volunteers.Methods
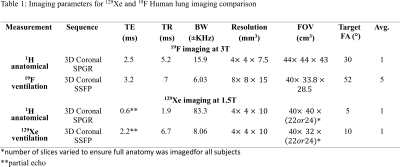
Three volunteers were imaged following informed consent using a protocol approved by the UK National research ethics committee. HP 129Xe images were acquired at 1.5T (GE HDx) with a flexible transmit/receive vest coil (CMRS, Brookfield, Wisconsin, USA). Fluorinated gas (80% C3F8 and 20% O2) imaging was performed at 3T (Philips Ingenia) with an elliptical transmit/receive quadrature birdcage coil (Rapid Biomedical). During ventilation and proton imaging, 1L of gas was inhaled from functional residual capacity to ensure equal lung inflation. Imaging sequences and parameters for all experiments are listed in Table 1. Each 19F scan was repeated a second time after the volunteer recovered while breathing the fluorinated gas mixture. The resulting images were averaged for higher subsequent SNR.
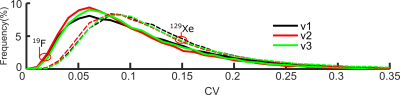
Images were segmented and median CV (as a measure of ventilation heterogeneity) calculated as previously described7. CV maps were generated by subsampling 129Xe images so that the image resolution was approximately equal to the reconstructed 19F image resolution (Table 1). A 3x3 kernel of 3.125 mm reconstructed pixel resolution (higher than the acquired resolution for both) was used to calculate local CV for every voxel within the ventilated lung volume.
Results
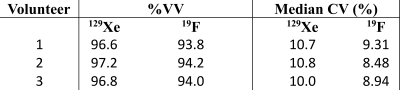
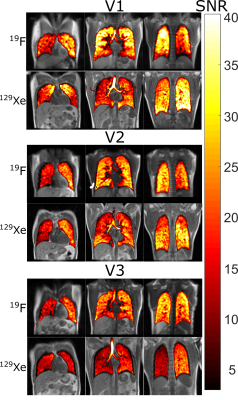
Figure 1 shows representative central slices from the healthy volunteers. Fluorinated gas images are blurred due to lower resolution and lower relative signal in the major airways can be observed. The %VV (Table 2) is lower in 19F measurements when compared to 129Xe by an average of 2%, while the median CV is on average 1.6% lower. From CV histograms in Figure 2 this change can be clearly observed with the shift of the CV distribution.Discussion and Conclusion
Although 19F and 129Xe images are analysed at the same reconstructed resolution, the CV from 19F imaging is consistently lower in all volunteers. The low CV from 19F is most likely due to the lower sampling resolution reducing signal variation in the 19F images. The %VV obtained with 129Xe imaging may potentially be replicated with 19F imaging, but here it was consistently lower by a small amount. This may be accounted for by lower observed signal in the inferior lung region and anterior slices, potentially from increased B1 in-homogeneity at 3T compared to 1.5T, which resulted in consistently lower 19F signal values for all volunteers. However, median CV and CV distribution also altered, and therefore may not be compared directly between images taken with the different gases. To further validate the results in this feasibility study, comparisons of fluorinated gas and 129Xe imaging at both 1.5T and 3T is underway, as well as repetition in patients with known respiratory conditions.
Acknowledgements
Doctoral program funding for Adam Maunder was partially provided by support from GE Healthcare Inc. and scholarships from the Natural Sciences and Engineering Research Council of Canada (NSERC) and University of Sheffield. Doctoral program funding for Paul J.C. Hughes was provided by support from GlaxoSmithKline and a scholarship from the University of Sheffield. This work was funded by the National Institute for health research (NIHR), Medical Research Council (MRC) and University of Sheffield Hyperpolarised Imaging Group - POLARIS. The views expressed in this abstract are those of the author and not necessarily those of NHS, NIHR, MRC or the Department of Health.References
1. S. J. Kruger, S. K. Nagle, M. J. Couch, Y. Ohno, M. Albert, and S. B. Fain, "Functional imaging of the lungs with gas agents," Journal of Magnetic Resonance Imaging, pp. 295-315, 2015.
2. Y. S. Tzeng, K. Lutchen, and M. Albert, "The difference in ventilation heterogeneity between asthmatic and healthy subjects quantified using hyperpolarized 3He MRI," J Appl Physiol (1985), vol. 106, pp. 813-22, Mar 2009.
3. M. Gutberlet, T. F. Kaireit, A. Voskrebenzev, F. Lasch, J. Freise, T. Welte, et al., "Free-breathing Dynamic 19F Gas MR Imaging for Mapping of Regional Lung Ventilation in Patients with COPD," Radiology, p. 170591, Oct 03 2017.
4. M. J. Couch, I. K. Ball, T. Li, M. S. Fox, S. L. Littlefield, B. Biman, et al., "Pulmonary ultrashort echo time 19F MR imaging with inhaled fluorinated gas mixtures in healthy volunteers: feasibility," Radiology, vol. 269, pp. 903-9, Dec 2013.
5. A. Maunder, N. J. Stewart, M. Rao, F. J. L. Robb, and J. M. Wild, "Steady-state Free Precession for Improved Signal to Noise in Lung Ventilation Imaging with 19F Perfluoropropane at 1.5 T," Proc. Intl. Soc. Mag. Reson. Med., vol. 25, p. 3318, 2017.
6. M. Couch, B. Blasiak, B. Tomanek, A. Ouriadov, M. Fox, K. Dowhos, et al., "Hyperpolarized and Inert Gas MRI: The Future," Molecular Imaging and Biology, vol. 17, pp. 149-162, 2015/04/01 2015.
7. P. J. C. Hughes, F. C. Horn, G. J. Collier, A. Biancardi, H. Marshall, and J. M. Wild, "Spatial fuzzy c-means thresholding for semiautomated calculation of percentage lung ventilated volume from hyperpolarized gas and 1 H MRI," J Magn Reson Imaging, Jul 06 2017.
Figures