1080
Pulmonary MRI Measurements of Ventilation Heterogeneity in Obstructive Lung Disease: Relationship to Oscillometry, Quality of Life and Disease Control1Robarts Research Institute, London, ON, Canada, 2Medical Biophysics, Western University, London, ON, Canada, 3Graduate Program in Biomedical Engineering, Western University, London, ON, Canada, 4School of Biomedical Engineering, Dalhousie University, London, ON, Canada
Synopsis
We measured ventilation heterogeneity in 100 patients (50 asthma, 50 COPD) with hyperpolarized 3He MRI, oscillometry and quality-of-life questionnaires. We showed that MRI-measured ventilation heterogeneity is significantly related to FOT-measured small airways resistance and worsened quality-of-life for asthma and COPD patients. We also showed that MRI-measured ventilation heterogeneity is significantly increased in asthmatic patients with poor disease control. This study directly demonstrates the relationships between 3He MRI ventilation heterogeneity with small airway dysfunction and patient quality-of-life.
Introduction
Ventilation heterogeneity is a hallmark finding of obstructive lung disease and has been measured using hyperpolarized 3He MRI and pulmonary function tests. Hyperpolarized 3He MRI has shown that obstructive lung diseases such as asthma and COPD are spatially heterogeneous, and this has been quantified by measuring regions of low 3He ventilation, or ventilation defects.1 However, the structural changes related to MRI ventilation defects are not yet fully understood. The forced oscillation technique (FOT) has been used to study structural changes in the lung related to ventilation heterogeneity by applying a multi-frequency pressure oscillation at the mouth to measure respiratory impedance, which is composed of respiratory system resistance (Rrs) and reactance (Xrs).2 Interestingly, FOT and 3He MRI have never been used together to study respiratory structure and function in asthma and COPD. By studying ventilation heterogeneity using MRI together with FOT, we may better understand how 3He MRI-measured heterogeneity is related to structural abnormalities, and the relationships to important clinical outcomes. We hypothesized that MRI ventilation defect percent (VDP) would be significantly related to FOT-measured respiratory system impedance and to patient quality of life.Methods
We evaluated 100 participants with obstructive lung disease (50 asthmatics, 50 COPD patients) who provided written informed consent to an ethics-board-approved protocol using hyperpolarized 3He MRI and oscillometry, as well as quality of life and disease control/exacerbation questionnaires. MRI was performed on a whole body 3T system (MR750 Discovery, GEHC, Milwaukee, WI) with broadband imaging capability. 3He MRI was acquired using a single-channel, rigid elliptical transmit/receive chest coil (RAPID Biomedical GmbH, Wuerzburg, Germany) and two-dimensional multi-slice fast spoiled gradient recalled echo sequence in a single breath-hold (acquisition time=10s; TR/TE/FA=3.8ms/1.0ms/7°; FOV=40×40cm2; BW=48.8kHz; matrix=128×80 (zero-padded to 128×128); 15 slices; slice thickness=15mm, 0gap). 3He gas was polarized to 30-40% polarization using a spin-exchange optical polarizer (Polarean Inc, Durham, NC).
Oscillometry was acquired by FOT using the TremoFlo C-100 Airwave Oscillometry System (Thorasys, Montreal CA). Validated questionnaires (Asthma Quality of Life Questionnaire, AQLQ, in asthma and the St. George’s Respiratory Questionnaire, SGRQ, in COPD) were used to evaluate patient quality of life. Disease control was evaluated using the Asthma Control Questionnaire (ACQ) in asthma and by monitoring exacerbations requiring hospitalization in COPD. Univariate relationships were evaluated using the Spearman correlation coefficient (ρ) and differences between groups were evaluated using independent samples t-tests with the Holm-Bonferroni correction to adjust for multiple comparisons. All statistical tests were performed using SPSS 24.0 (IBM, Armonk, NY).
Results
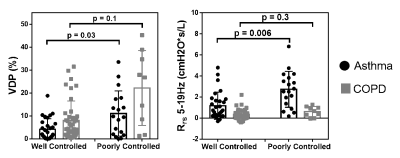
Figure 1 shows 3He MRI for 3 representative subjects with asthma, and 3 subjects with COPD with increasing ventilation heterogeneity and Rrs and Xrs. The relationships between MRI VDP and FOT-measured impedance are also shown. VDP was significantly related to FOT-derived small-airways resistance (Rrs5-19Hz) in both asthma (ρ=0.5, p<0.001) and COPD (ρ=0.4, p=0.001) and VDP was related to the total respiratory impedance only in asthma (Rrs5Hz: ρ=0.3, p=0.02; Xrs5Hz: ρ=-0.5, p<0.001). Figure 2 shows the relationships between MRI VDP and FOT-measured impedance with quality of life questionnaires in asthma and COPD. MRI VDP and FOT-derived small-airway resistance (Rrs5-19Hz) were significantly related to quality of life scores in asthma (ρ=-0.3, p=0.04; ρ=-0.3, p=0.04) and COPD (ρ=0.4, p=0.008; ρ=0.4, p=0.004). Figure 3 shows MRI VDP and FOT-measured impedance in subjects with good disease control (no exacerbations) and poor disease control (with exacerbations). In asthma, patients with poor disease control had significantly higher VDP (p=0.03) and small-airways resistance (p=0.006). There was no significant difference in VDP (p=0.1) or small-airways resistance (p=0.3) between COPD patients with good or poor disease control. In asthma, patients with poor control also had significantly increased respiratory system resistance (Rrs5Hz: p=0.01) and reactance (Xrs5Hz: p=0.03).Discussion and Conclusion
This study provides strong evidence to support the relationship between MRI ventilation heterogeneity and small airways dysfunction in obstructive lung disease. Importantly, we also showed that MRI-measured ventilation heterogeneity is related to FOT-measured respiratory system impedance and both are related to disease control and quality of life. This study also provides evidence that MRI measurements of ventilation heterogeneity acquired under breath-hold conditions reflect mechanical changes that are observed during tidal breathing. We showed for the first time that FOT-measured impedance is related to MRI ventilation defects, and both are related to quality of life in patients with obstructive lung disease.Acknowledgements
No acknowledgement found.References
1. Kirby et al. Acad Radiol, (2012).
2. Oostveen et al. Eur Respir J, (2003).
Figures
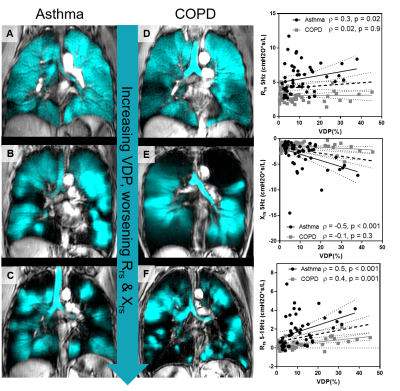
Figure 1. 3He MRI for 3 representative subjects with asthma, and 3 subjects with COPD with increasing ventilation heterogeneity and Rrs and Xrs.
From top to bottom: asthma: (A) VDP=5%, (B) VDP=10%, (C) VDP=17%. COPD: (D) VDP=8%, (E) VDP=11%, (F) VDP=32%. The relationships between VDP and FOT-measured impedance are also shown. (Top) Rrs 5Hz (asthma: ρ=0.3, p=0.02; COPD ρ=0.02, p=0.9), (middle) Xrs5Hz (asthma: ρ=-0.5, p<0.001; COPD ρ=-0.1, p=0.3), (bottom) Rrs5-19Hz (asthma: ρ=0.5, p<0.001; COPD ρ=0.4, p=0.001).
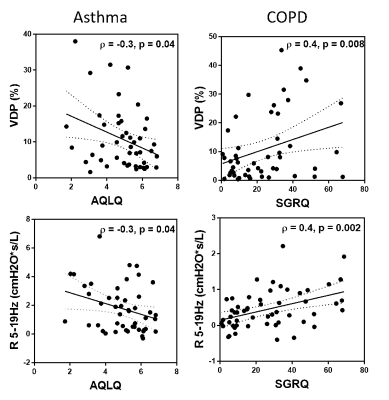
Figure 2.
Top: Univariate relationships between MRI VDP and quality of life questionnaires in asthma (AQLQ: ρ=-0.3, p=0.04) and COPD (SGRQ: ρ=0.4, p=0.008). Bottom: Univariate relationships between FOT-measured small-airway resistance and quality of life questionnaires in asthma (AQLQ: ρ=-0.3, p=0.04) and COPD (SGRQ: ρ=0.4, p=0.002).