1078
Repeatability of ventilation and perfusion impairment assessed with matrix pencil decomposition MRI and lung function in children with cystic fibrosis1Division of Radiological Physics, Department of Radiology, University of Basel Hospital, Basel, Switzerland, 2Department of Biomedical Engineering, University of Basel, Basel, Switzerland, 3Pediatric Respiratory Medicine, Department of Pediatrics, Inselspital, Bern University Hospital, University of Bern, Bern, Switzerland, 4Departement of Diagnostic, Interventional and Paediatric Radiology, Inselspital, University Hospital Bern, Bern, Switzerland
Synopsis
This study examines the repeatability of functional lung MRI using matrix pencil decomposition and lung function tests with multiple breath washout technique in children with cystic fibrosis and age-matched healthy controls. We found a good degree of the agreement between outcomes measured on two consecutive days in both groups. Furthermore, a strong correlation between functional MRI and global ventilation inhomogeneity index from multiple breath washout was observed. The results of this study highlight the potential of matrix pencil decomposition MRI for the assessment of disease progression in cystic fibrosis
Purpose
Cystic fibrosis (CF) can be monitored by the application of imaging and lung function modalities such as the nitrogen multiple breath washout (N2-MBW) technique.1,2 Although not established as a gold-standard, MRI can be used a non-invasive and radiation free technique for both structural and functional assessment of the lung in CF. Recently, pulmonary functional matrix pencil (MP) decomposition MRI3 (a derivative of Fourier decomposition MRI4) was shown to provide complementary outcome measures to N2-MBW for the diagnostic monitoring in CF.5 In the current study we examined short term variability (two measurements within 24 hours) of ventilation and perfusion impairment detected in CF children and healthy controls using MP MRI and N2-MBW.
Methods
Study population and design
Twenty-three children with CF children (range: 6-18 years, mean age: 13.5 years, females, 6 males) were enrolled into the study. Twelve healthy controls (range: 6-17 years, mean age: 11.9 years , 5 females, 7 males) had neither a history of chronic lung disease nor acute respiratory infection in the 4 weeks prior to the investigations. All subjects underwent MRI, spirometry and N2-MBW examinations on two consecutive days. The study was approved by the local Ethics Committee and written informed consent obtained from parents and participants older than 14 years.
MR data acquisition and analysis
Functional and morphological MRI was performed on a 1.5T clinical MR-scanner (Aera, Siemens Healthineers, Germany) without the administration of contrast agent. Lung function was assessed with MP MRI, yielding fractional ventilation (FV) and relative perfusion (Q) images. All scans were performed without sedation, the functional MRI was performed in free breathing. Parents were allowed to accompany children in the scanner cabin during imaging. The signal distributions on the segmented FV and Q images were analyzed to estimate threshold values indicating functional impairment equal to 0.75 of median value from the voxel distributions.5 Values of relative impaired ventilation (RFV) and relative perfusion (RQ) were calculated for every subject.
Lung function testing
N2-MBW washout was performed with an unmodified device (Exhalyzer D, Eco Medics AG, Switzerland) according to consensus.6 Primary outcome was the lung clearance index (LCI), calculated as cumulative expired volume over functional residual capacity, for global ventilation inhomogeneity. Secondary outcomes was the functional residual capacity.
Statistical analysis
Agreement over visits from MRI and lung function
indices was studied by calculating intra-class correlation (ICC) coefficients (ICC>0.6 - good, ICC>0.8 - excellent).
Wilcoxon signed rank test was used to compare distributions of variables between visits. Correlations between functional indices from MRI
and lung function were calculated with the Spearman's correlation coefficients. P-values <0.05 were considered statistically
significant.
Results
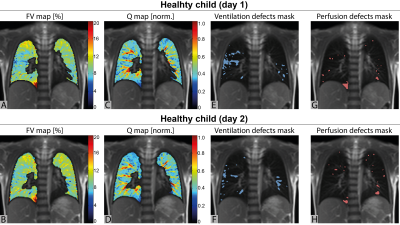
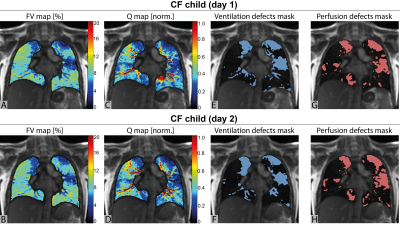
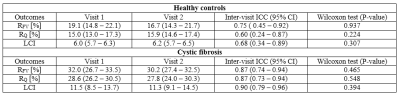
Figure 1 and 2 show exemplary functional lung images obtained during both visits in a healthy subject and a CF child, respectively. Fractional ventilation impairment (RFV) and perfusion impairment (RQ) was significantly higher in CF patients compared to healthy controls on both visits. In both groups, no significant difference in RFV, RQ or LCI between both visits was found (Table 1). The agreement between MRI and N2-MBW outcomes in both visits calculated using inter-class correlation was
higher for CF participants than for healthy children (Table 1).
In CF patients, there was a strong correlation between RFV and LCI at visit 1 and 2, r=0.75 (P<0.001) and r=0.67 (P<0.001), respectively. RQ showed a significant, excellent correlation with LCI
at visit 1: r=0.79 (P<0.001), and visit 2 r=0.59 (P=0.004).
Discussion and Conclusion
We observed a good short term repeatability of the detection of fractional ventilation and perfusion impairment measured with MP MRI and lung function. The degree of the agreement between both visits was good in both groups. Similarly to the previous study5, we found strong correlations between functional parameters from MRI and multiple breath washout technique.
Routine application of MP MRI is possible without the need
for contrast agent administration, exposure to radiation or breathing maneuvers. The whole examination can be performed in a clinically acceptable time of less than 10 minutes using commercially available MR equipment.
In summary, MP MRI is feasible and repeatable in children with CF and in healthy controls. Thus, we assume, that the outcomes of MP MRI could be used as a biomarker for the detection of changes
in lung function impairment in lung disease.
Acknowledgements
Swiss National Science Foundation; Grant number: SNF 320030_149576.References
1. Ramsey KA, Rosenow T, Turkovic L, et al. Lung clearance index and structural lung disease on computed tomography in early cystic fibrosis. Am J Respir Crit Care Med 2016; 193: 60–67
2. Eichinger M, Optazaite DE, Kopp-Schneider A, et al. Morphologic and functional scoring of cystic fibrosis lung disease using MRI. European journal of radiology. 2012;81(6):1321-9.
3. Bauman G, Bieri O. Matrix pencil decomposition of time-resolved proton MRI for robust and improved assessment of pulmonary ventilation and perfusion. Magn Reson Med 2017; 77: 336–342.
4. Bauman G, Puderbach M, Deimling M, et al. Non-contrast-enhanced perfusion and ventilation assessment of the human lung by means of Fourier decomposition in proton MRI. Magn Reson Med 2009; 62: 656–664.
5. Nyilas S, Bauman G, Sommer G, et al. Novel magnetic resonance technique for functional imaging of cystic fibrosis lung disease. Eur Respir J 2017 doi: 10.1183/13993003.01464-2017 [Epub aread of print]
6. Robinson PD, Latzin P, Verbanck S, et al. Consensus statement for inert gas washout measurement using multiple- and single- breath tests. The European respiratory journal. 2013;41(3):507-22. 5.
Figures