1055
Transient intrinsic torsional shear wave propagation demonstrates a difference in Left Ventricular Myocardial stiffness between volunteers and patients with HFpEF1King's College London, London, United Kingdom, 2Guys and St Thomas' NHS Trust, London, United Kingdom, 3Universitat Ramon Llull, Barcelona, Spain, 4Philips Healthcare, Guildford, United Kingdom
Synopsis
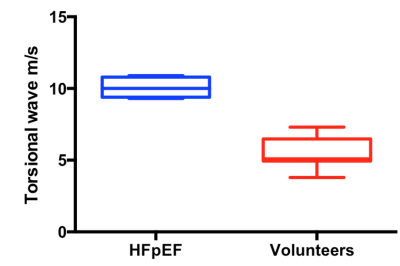
Heart Failure with preserved Ejection Fraction is common, associated with high morbidity and mortality, and is challenging to diagnose. We have developed a novel patient friendly non-invasive technique to quantify myocardial stiffness using transient MR Elastography. Aortic valve closure results in the propagation of a transient shear wave through the myocardium. Torsional wave propagation can be visualised using a 1D pencil beam navigator positioned longitudinally along the myocardial septum, using four breath holds each 15 seconds. Providing a temporal resolution of 0.3ms, we observe increased myocardial stiffness in HFpEF patients compared to healthy volunteers (torsional speed 5.5 ± 1.1 m/s in volunteers and 10.0 ± 0.7 m/s in Patients; stiffness 36 ± 12.0 kPa and 108 ± 15.2 kPa, respectively) .
Background
Heart Failure with preserved Ejection Fraction (HFpEF) is increasingly common and associated with high morbidity and mortality (1). HFpEF is characterised by increased myocardial stiffness and our preliminary data using transient MR-Elastography utilizing the aortic valve closure as an intrinsic source for the generation of shear waves, has validated that stiffness can be measured using MRI (2). Our previous approach similarly used a 2D pencil beam to capture the wave at a single snapshot around valve closure. While this enables the characterization of wavelength, the stiffness could not be directly estimated without capturing the propagation of the shear wave. In this work, we further developed the method to enable the visualization of the torsional wave propagation (3) through the myocardium at temporal resolutions of 0.3ms acquired within 4 consecutive breath-holds.Methods
This study has 3 parts: sequence development, validation of wave speed measurements in phantom models and a patient/volunteer study (n=15).
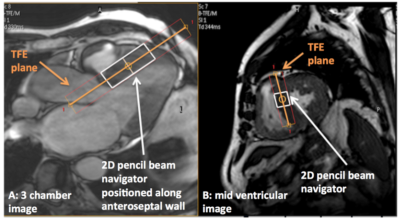
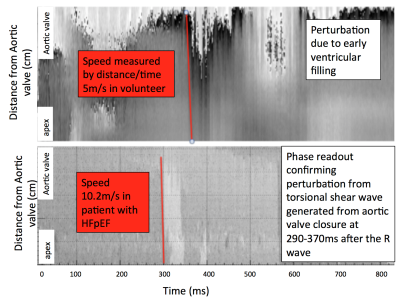
The sequence is ECG-triggered and consists of a block of ~40 consecutive 2D pencil beam shots (30mm, 80mm lengths, 20ms duration) played throughout a single R-R interval. Image shots in subsequent R-R intervals are time-shifted relative to the QRS-start. With typically 35-40 shots per R-R interval (depending on the person’s heart rate), 15sec breath hold time, and 4 repetitive breath holds, a temporal resolution of (20ms/[4*15]) 0.3ms can be achieved. The total number of consecutive image shots covers ~80% of the cardiac cycle, with the rest as a time buffer and allowing for patients with different heart rates to be scanned. Motion sensitisation is possible in all three orthogonal directions (fMEG=160 Hz) allowing to uniquely select the torsional wave. Unlike the flexural and compressional wave components, which are biased in their speed by geometry, the torsional wave component propagates unbiased and can hence be used to infer the intrinsic properties of the material. The navigator is positioned (figure 1) along the anteroseptal wall of the myocardium. The entirety of all time-reordered phase data provides a space-time image that allows visualising the propagation of shear waves within the imaging volume. Fitting a straight line to the perturbation that correlates to the time point of aortic valve closure yields the unbiased shear wave’s speed.
Results
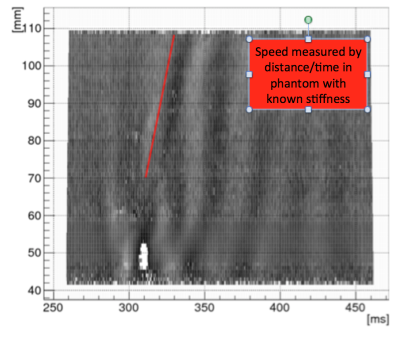
Phantom experiments using known material stiffness demonstrated that the sequence allows to properly capture shear wave propagation at high temporal resolution (figure 2) with stiffness measured as distance/time, and corresponding to the true material stiffness. The compressional wave is seen by a vertical line due to its elevated speed. 3D finite-element simulations confirmed the existence of a torsional wave generated by aortic valve closure propagating at a speed that corresponded to the true shear stiffness of the myocardium used for the simulation.
Torsional shear waves were observed in ten healthy volunteers and five patients with HFpEF between 290-370ms after the R wave (figure 3), corresponding to valve closure time. The mean wave speed was 5.5 ± 1.1 m/s in volunteers and 10.0 ± 0.7 m/s in patients (p <0.0001, figure 4), resulting in shear modulus estimates of 36 ± 12.0 kPa and 108 ± 15.2 kPa respectively.
Four of the patients have invasive pressure volume loop studies that confirmed increased LV chamber stiffness with prolonged tau (τ), the isovolumic relaxation constant at 55-60ms and LVEDP at rest of 18-20mmHg.
Discussion
This innovative sequence design has allowed us to demonstrate increased myocardial stiffness in patients with HFpEF by measuring the unbiased torsional wave that is in keeping with the invasive measures of LV chamber stiffness. Our phantom and 3D finite element simulations have confirmed the validity of our technique, in agreement with the theory for wave propagation in hollow cylinders and opens the gateway to measure cardiac biomechanics non-invasively without the need for external transducers. The sequence does not rely on prior knowledge of exact valve closure time, which would require additional scans and changes during the scan with the heart rate. Collectively, this has resulted in a sequence that is patient friendly, requires no external vibration, is easy tolerated and can be applied to any patient in sinus rhythm.Conclusion
We have successfully developed and applied a new patient friendly technique to quantify myocardial stiffness in vivo from torsional shear waves generated by aortic valve closure, not requiring any external transducers. We have shown that patients with HFpEF have increased myocardial stiffness compared to volunteers, in keeping with our invasive pressure volume loop studies. This method has significant potential to become an important diagnostic tool for the early detection of pathologically altered myocardial stiffness that will facilitate better treatment resulting in improved patient outcomes. Importantly, measured stiffness values agree with those expected from simulations, i.e. ~30kPa at end systole.Acknowledgements
Radiographers at King's College LondonReferences
1 Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006; 355:251–9.
2 Webb J, Holub O, Clough R et al. Using intrinsic Cardiac Shear Waves to measure Myocardial Stiffness: Initial results on a Patient Cohort with Heart failure with preserved Ejection Fraction. Proc. Intl. Soc. Mag. Reson. Med. 2016;24:0412.
3 Webb J, Runge JH, Martorell J et al. Using transient intrinsic torsional shear wave propagation to measure Left Ventricular Myocardial stiffness with a 2D pencil beam navigator at 0.5ms temporal resolution: Initial results from phantom studies and volunteers. Proc. Intl. Soc. Mag. Reson. Med. 2017;25:0636.
Figures