1042
Intravoxel Incoherent Motion (IVIM) Imaging in Human Achilles Tendon1Biomedical Engineering, Stony Brook University, Stony Brook, NY, United States, 2Radiology, Stony Brook University Hospital, Stony Brook, NY, United States
Synopsis
Clinically, Achilles tendon (AT) rupture accounts for 40-60% of all operative tendon repairs. AT microcirculation plays a crucial role in the progression of tendinopathy and tendon repair. In this study a novel ste-RESOLVE IVIM protocol was developed to image AT microcirculation. Healthy participants were imaged pre- and post-exercise, and exercised induced increases in blood volume and blood flow were observed. AT tendinopathy patients exhibited greater baseline blood volume and blood flow when compared to healthy participants. For the first time, a robust MRI-based technique was developed to investigate the role of Achilles tendon microcirculation in tendinopathy.
Introduction:
Clinically, Achilles tendon (AT) rupture accounts for 40-60% of all operative tendon repairs, with 75% due to sports-related activities1. Conventional MR images exhibit poor contrast and specificity in delineating low-grade tendon injuries necessitating the development of novel AT imaging techniques2. AT microcirculation plays a crucial role in the progression of tendinopathy and tendon repair3. However, tendon perfusion rate is too low to be reliably quantified clinically. Intravoxel incoherent motion (IVIM) MRI has been utilized to study skeletal muscle hemodynamics4 but its application to the AT is a challenging due to the short T2/T2* values of tendons (~7ms) and the requirement of long echo time (TE) (~50-80ms) . In this study, utilizing a previously developed stimulated-echo based short TE (~10-20ms) tendon diffusion protocol (ste-RESOLVE)5, AT microcirculation and hemodynamic changes were evaluated in healthy participants at baseline and after exercise and in tendinopathy patients at baseline.Methods:
Ten healthy participants and six Achilles tendinopathy patients were recruited for this IRB approved study on a Siemens Prisma 3T magnet using a flexible 4-channel coil. A novel approach of combining stimulated-echo diffusion and readout-segmented multi-shot EPI (ste-RESOLVE) was developed and the magic angle effect was exploited to increase tendon T2/T2*. The sequence parameters for ste-RESOLVE IVIM were: FOV of 160×100mm2; matrix of 80×50; 8 axial slices with thickness of 6mm and 100% separation; TR/TE of 2200/20ms; readout segmentation factor of 7 with echo spacing of 0.3ms; iPAT2; stimulated echo duration of 200ms; b-values of 0, 20, 40, 60, 80, 120, 200, 400, and 600s/mm2. The total acquisition time was ~8min for 9 diffusion weightings. Seven healthy participants were imaged at baseline and after 5 minutes of stressful heel-raise exercise outside of the scanner. Three additional healthy participants and six tendinopathy patients were imaged only at baseline. To compare healthy participants and Achilles tendinopathy patients the AT was segmented into three regions (proximal, medial, and distal). The tendon diffusion coefficient (D), pseudo-diffusion coefficient (D*), and perfusion fraction (fp) were calculated using a standard bi-exponential fit.Results:
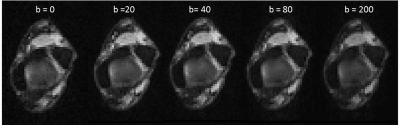
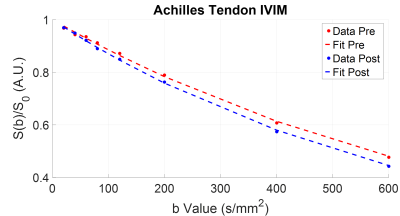
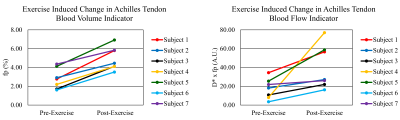
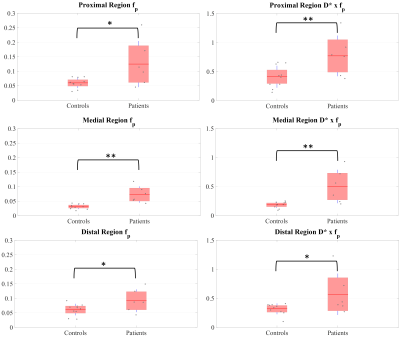
Figure 1 shows diffusion-weighted images acquired with the ste-RESOLVE IVIM sequence (images with b-values of 400 and 600s/mm2 not shown). Figure 2 demonstrates the IVIM signal profile at pre- and post-exercise for a healthy participant. Ladder plots for blood volume and blood flow sensitive parameters (fp and D*×fp respectively) are displayed in Fig. 3. As expected, all subjects exhibited increased blood flow and blood volume following exercise. The pre-exercise measured fp and D*×fp were 2.81±1.09% and 17.45±10.81 respectively. The post-exercise measured fp and D*×fp were 4.96±1.23% and 40.52±23.27 respectively. The relative increase in tendon blood volume and tendon perfusion was 87.11% and 227.41%, respectively. Box plots of fp and D*×fp in the three segmented regions for healthy participants and Achilles tendinopathy patients at baseline are shown in Fig. 4. The average fp in the proximal, medial, and distal regions was 0.06±0.02, 0.03±0.01, and 0.06±0.02 for healthy subjects, and 0.12±0.08, 0.07±0.03, and 0.09±0.04 for tendinopathy patients. The average D*×fp in the proximal, medial, and distal regions was 0.41±0.19, 0.18±0.05, and 0.32±0.09 for healthy participants, and 0.77±0.35, 0.50±0.29, and 0.57±0.36 for tendinopathy patients. A significant difference (un-paired, two-tailed t-test, p-value<0.05) was found between healthy participants and tendinopathy patients for both fp and D*×fp in all three regions.Discussion:
This study evaluated the feasibility and robustness of a ste-RESOLVE IVIM protocol that can be used to investigate the microvascular circulation in AT. An increase in blood volume and blood flow was observed after exercise and is consistent with the expected exercise-induced tendon hemodynamics changes as observed in other studies6. Increased AT blood volume and blood flow in tendinopathy patients has been associated with painful tendon lesions but is not associated with tendon repair7-9. The elevated fp and D*×fp detected in patients suffering from Achilles tendinopathy suggests the proposed method can detect tendinopathy induced vasculature changes.Conclusion:
For the first time, a robust MRI-based technique was developed to investigate the role of Achilles tendon microvasculature in tendinopathy. The novel ste-RESOLVE IVIM approach has the potential to monitor tendinopathy progression and assess the risk of tendon rupture.Acknowledgements
No acknowledgement found.References
1. Järvinen TAH, Kannus P, Maffulli N, Khan KM. Achilles Tendon Disorders: Etiology and Epidemiology. Foot and Ankle Clinics. 2005;10(2):255-266.
2. Reiman M, Ciara Burgi, Eileen Strube, et al. The Utility of Clinical Measures for the Diagnosis of Achilles Tendon Injuries: A Systematic Review With Meta-Analysis. Journal of Athletic Training. 2014;49(6):820-829.
3. Fenwick SA, Hazleman BL, Riley GP. The vasculature and its role in the damaged and healing tendon. Arthritis Research & Therapy. 2002;4(4):252.
4. Filli L, Boss A, Wurnig MC, Kenkel D, Andreisek G, Guggenberger R. Dynamic intravoxel incoherent motion imaging of skeletal muscle at rest and after exercise. NMR in Biomedicine. 2015;28(2):240-246.
5. He X, Wengler K, Sacher A, et al. Diffusion Tensor Imaging of Human Achilles Tendon by Stimulated Echo RESOLVE (ste-RESOLVE) Paper presented at: ISMRM 2016; Singapore.
6. Kubo K, Ikebukuro T, Tsunoda N, Kanehisa H. Noninvasive measures of blood volume and oxygen saturation of human Achilles tendon by red laser lights. Acta Physiol (Oxf). 2008;193(3):257-264.
7. Astrom M, Rausing A. Chronic Achilles tendinopathy. A survey of surgical and histopathologic findings. Clin Orthop Relat Res. 1995(316):151-164.
8. Kvist M, Jozsa L, Jarvinen MJ, Kvist H. Chronic Achilles paratenonitis in athletes: a histological and histochemical study. Pathology. 1987;19(1):1-11.
9. Yu JS, Popp JE, Kaeding CC, Lucas J. Correlation of MR imaging and pathologic findings in athletes undergoing surgery for chronic patellar tendinitis. AJR Am J Roentgenol. 1995;165(1):115-118.
Figures