1001
Higher-Resolution Prostate Diffusion MRI with Minimized Echo Time using Eddy Current Nulled Convex Optimized Diffusion Encoding (ENCODE)1Department of Radiological Sciences, University of California, Los Angeles, Los Angeles, CA, United States, 2Department of Bioengineering, University of California, Los Angeles, Los Angeles, CA, United States
Synopsis
Higher-resolution prostate DWI has the potential to improve prostate cancer diagnosis, but suffers from additional SNR reduction due to increased TE at longer EPI readouts for current diffusion encoding schemes. In this work, we evaluated the newly proposed Eddy Current Nulled Convex Optimized Diffusion Encoding to achieve eddy-current-free diffusion encoding with minimized TE for prostate diffusion MRI using standard and higher-resolution protocols. The ENCODE higher-resolution protocol achieves higher scores for image sharpness and contrast compared to standard-resolution prostate DWI.
Introduction
Diffusion-weighted MRI (DWI) is a key component of prostate multi-parametric MRI. Monopolar spin echo (MONO) is the standard DWI encoding scheme, but suffers from eddy current induced distortion artifacts. Twice refocused spin echo (TRSE) DWI effectively reduces eddy current artifacts, but increases TE and reduces SNR compared to MONO. Higher-resolution prostate DWI has potential to improve prostate cancer diagnosis1, but suffers from additional SNR reduction due to increased TE at longer EPI readouts for current encoding schemes (MONO or TRSE). Recently, Eddy Current Nulled Convex Optimized Diffusion Encoding (ENCODE) has been developed to null eddy current effects and minimize TE.2 The objective of this study was to evaluate ENCODE versus MONO and TRSE for prostate DWI in terms of eddy current artifacts, SNR, ADC, and diagnostic image quality (sharpness and contrast) at standard- and higher-resolution imaging protocols.
Methods
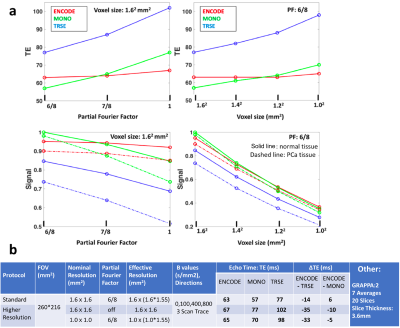
Prostate DWI using ENCODE/MONO/TRSE were evaluated for: 1.Standard-resolution protocols with 1.6x1.6mm2 nominal resolution (RN) and partial Fourier factor (PF) = 6/8,3 and 2.Higher-resolution protocols with modified RN (up to 1.0x1.0mm2) and PF (6/8 or off). Parameters are in Figure 1. Effective resolution (RE) of each protocol was estimated by RE=RN * blurr(PF), where blurr(PF=6/8) =1.55.4
Theoretical Comparison: ENCODE, TRSE and MONO waveforms were generated to compare their TE. Assuming normal prostate T2,norm = 120ms and ADCnorm = 1200*10-6mm2/s, prostate cancer (PCa) T2,PCa = 70ms and ADCPCa = 800*10-6mm2/s,5,6 SE-DWI signals were compared using S(TE,b)=M0*exp(-TE/T2)*exp(-b*ADC)*RN.
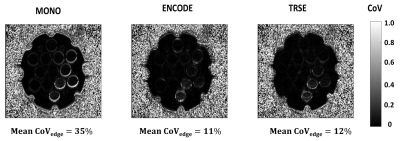
Phantom Imaging: A standardized diffusion phantom was imaged at 3T (Prisma, Siemens, GMax=76mT/m) using prostate DWI protocols (Figure 1b). To evaluate eddy-current induced distortion artifacts, voxel-wise coefficient of variation (CoV) was calculated across diffusivity maps of each diffusion direction and compared.
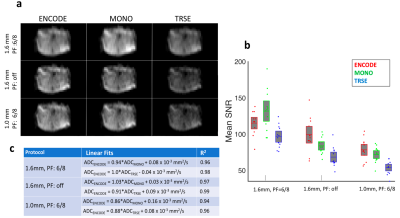
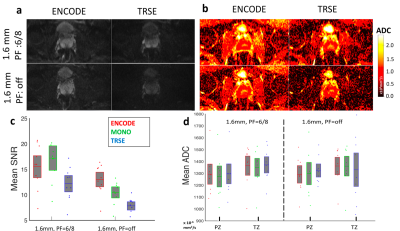
Prostate Imaging: In an IRB-approved and biosafety-approved study, one ex-vivo prostate specimen and 10 healthy subjects (age 27±3 years) were imaged using identical protocols as phantom study. Ex-vivo Prostate Imaging: SNR analysis: Prostate DWI at b=800s/mm2 were acquired 7 times to calculate SNR maps for each sequence. ADC analysis: Linear correlation of ADC from each sequence were investigated using mean ADC from 12 regions within the prostate. In-vivo Prostate Imaging: SNR analysis: SNR maps were computed from 7 repetitions and mean SNR of the whole prostate were compared among sequences. ADC analysis: Mean ADC from the prostate transition zone (TZ) and peripheral zone (PZ) were measured and compared among sequences. Image Quality Analysis: Two radiologists scored the ENCODE and TRSE DWI/ADC (blinded and randomized) in terms of image sharpness (IS) and contrast (CA) on a 5-point Likert scale (1:worst,5:best) for standard- and higher-resolution protocols. Statistical Analysis: Differences among ENCODE/TRSE/MONO prostate DWI were tested using one way analysis of variance; P<0.05 was considered significant.
Results
Theoretical Comparison: ENCODE achieved substantially lower TE than TRSE, especially for higher-resolution protocols (up to 35ms shorter) (Figure 1), which resulted in 25%-40% higher expected prostate signal versus TRSE.
Phantom Imaging: ENCODE achieved comparable eddy current nulling performance as TRSE in prostate DWI protocols, while eddy current induced artifacts were evident on MONO (Figure 2).
Prostate Imaging: ADC: Ex-vivo imaging shows ENCODE ADC within prostate were consistent with TRSE/MONO across all protocols using linear regression (Figure 3). Standard-resolution in-vivo results show that ENCODE ADC in the prostate PZ and TZ were similar to MONO and TRSE (Figure 4). For higher-resolution in-vivo imaging, ENCODE and MONO ADC were consistent with each other, while TRSE ADC had increased variation. SNR: By minimizing TE, ENCODE achieved 20%-60% higher SNR than TRSE in ex-vivo (Figure 3b) and in-vivo prostate DWI (Figure 4c), with the most pronounced gain for higher-resolution protocols. Image Quality: For in-vivo imaging, the ENCODE higher-resolution protocol (1.6x1.6mm2, PF=off) had the highest scores for both IS and CA: ISENCODE,High=4.5±0.5, ISENCODE,standard=3.0±0.6, ISTRSE,standard=2.2±0.4, ISTRSE,High=1.7±0.6; CAENCODE,High=4.3±0.7, CAENCODE,standard=3.5±0.6, CATRSE,standard=2.7±0.4, CATRSE,High=1.3±0.4. Representative images are shown in Figure 5.
Discussion
ENCODE prostate DWI achieves comparable eddy current nulling performance as TRSE, while substantially decreasing TE and significantly increasing prostate tissue SNR. The advantages in decreasing TE and increasing SNR are most pronounced for the higher-resolution protocols. Prostate ADC quantification using ENCODE is consistent with MONO for both standard- and higher-resolution protocols, while TRSE ADC was found to have increased variation at higher resolution, mostly likely due to the SNR loss caused by elongated TE. The ENCODE higher-resolution protocol (1.6x1.6mm2, PF=off) achieved higher scores for image sharpness and contrast compared to standard-resolution prostate DWI, and could potentially improve prostate cancer diagnosis.Conclusion
ENCODE generates eddy-current-free diffusion encoding with minimized TE for prostate DWI at standard and higher-resolution protocols. The improvement in image quality using higher-resolution ENCODE prostate DWI can potentially improve clinical prostate cancer diagnosis.Acknowledgements
This study was supported in part by the UCLA Departments of Radiological Sciences and Bioengineering, The authors thank the David Geffen School of Medicine at UCLA and the UCLA Magnetic Resonance Research Labs for research support .References
- Medved M, et al., Am J Roentgenol 2014 203:1, 85-90
- Aliotta E, et al., Magn Reson Med 2017;doi:10.1002/mrm.26709
- Tan N, et al., Am J Roentgenol 2015; 205: W87-92
- Chaimow D, et al. bioRxiv 2017; https://doi.org/10.1101/097154
- Dregely I, et al. Magn Reson Med 2016; 76: 1720–1729
- Woodfield C, et al. Am J Roentgenol. 2010; 194: W316-22.
Figures