0917
Time-resolved dynamic contrast enhanced MR imaging of the pulmonary vasculatures and parenchyma using Fat-sat DISCO with Gadobutrol1Radiology, Seirei Hamamatsu General Hospital, Hamamatsu, Japan, 2Global MR Applications and Workflow, GE Healthcare, Hino, Japan, 3Global MR Applications and Workflow, GE Healthcare, Madison, Japan
Synopsis
Fat-sat DISCO is modified version of DISCO, based on LAVA with view-sharing, which can be used for dynamic contrast MR imaging with high temporal resolutions. Gadobutrol has higher concentration of Gadolinium and its single bolus injection might induce T2 shorting effects. Simultaneous bolus injection of Gadobutrol and saline may suppress T2 shorting effects and will facilitate enhancement on T1-weighted imaging. Using fat-sat DISCO with simultaneous bolus injection of Gadobutrol and saline, dynamic contrast MR imaging of the lung can steadily provide selective visualization of pulmonary vasculatures and parenchymal enhancement.
Introduction
Dynamic contrast pulmonary MR imaging with high temporal resolution can provide information of selective vascular anatomy and parenchymal perfusion. Currently, we used a modified version of Differential Sub-sampling with Cartesian Ordering1 (F-DISCO), which is based on 3D T1-weighted imaging, LAVA with Spec IR using adiabatic pulse for fat saturation and apparent temporal resolution for one phase covering the thorax can be set less than two seconds. Gadobutrol (Gd-DO3A-butrol, Bayer HC) may induce strong T2 shorting effects with bolus injection due to higher concentration of Gadolinium. Thus, simultaneous injection of gadobutrol and saline can be performed for dilution. Accordingly, the purpose was to evaluate feasibility of dynamic enhanced MR imaging for evaluation of the pulmonary vasculatures and parenchyma using fast imaging technique F-DISCO with simultaneous injection of Gadobutrol and saline.
Materials and Methods
The current study was approved by the institutional review board (IRB) in our hospital and informed consent was obtained from each patient. Population: 30 patients who underwent dynamic contrast MR imaging for the evaluation of the thorax were included (men:women=20:10 , mean age 45 years old). MRI: MR imaging was performed on a 3T magnet (Discovery 750, GEHC) with 32 channel phased array multicoil. After localization, dynamic contrast enhanced MR imaging was performed with F-DISCO (a modified version of DISCO), with following imaging parameters; TR 2.6ms, TE 0.9ms, 70-88 slices, 25-30phases, slice thickness 3-5mm with 50% overlap, FOV 35-40cm, Matrix 256x224-200, SecIR (adiabatic pulse) for fat saturation. Apparent temporal resolution per phase was 1.4-1.9sec. MR contrast medium and Injection method: MR contrast medium Gadobutrol (Gd-BT-DO3A 1.0mmol/mL, 0.1mmol/kg, Bayer HC) was injected through cubital vein at an injection rate of 1ml/sec with simultaneous injection of saline at the rate of 2ml/sec). Two second after injection of Gd-chelate, serial dynamic MR images were obtained with possible 20-30 seconds’ breath holding followed by quiet free breathing. Evaluations: Subjective: With selection of optimal phase for visualization of following structure as Right ventricle, Pulmonary artery (main, distal), Pulmonary parenchyma, Pulmonary veins (main), Ascending Aorta- Aortic arch, image quality (overall, homogenous SI for each structure), artifacts (blurring, noise), degree and homogeneity of fat signal suppression (mediastinum, supraclavicular area) were evaluated using a five point scale (5 excellent, no artifact-1 poor, artifacts). And in the selected phase for each structure, visualization of 28 segments of the vasculatures in each patient was evaluated using a five point scale (5 excellent-1 not visualized, poor): the pulmonary arteries, veins and the aorta. Homogeneous enhancement in the pulmonary parenchyma was evaluated and recognition of Minor fissure in the right lung was also evaluated using a five point scale (5 excellent- 1 poor, not visualized). Positive (Visualized) and negative was regarded as for sore of 4 and 5, and for that of 1 or 2, respectively. Three observers independently evaluated features and difference in positive and negative documents were resolved with consensus. Objective: Signal intensity changes in each structure for serial dynamic contrast images.Results
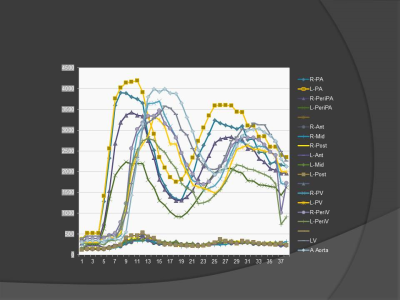
In all cases, image qualities for pulmonary vasculatures were good and artifacts were not prominent (Fig 1). All 28 segments of pulmonary vasculatures were well visualized (Figs 2-4A). Homogenous enhancement of the pulmonary parenchyma could be observed in all cases and minor fissure in the right lung could be recognized as low intensity area (Fig4B). Fat saturation was accomplished in the mediastinum but, in supraclavicular areas, fat saturation was inhomogenously made (Fig 4B). Representative signal intensity change in various regions (Fig 5). Perfusion of the pulmonary parenchyma could be recognized in all patients.Discussion
The current study demonstrated fast dynamic contrast imaging with high temporal resolutions could constantly provide vascular anatomy as well as perfusion of pulmonary parenchyma. The contrast media utilized in the current study was Gadobutrol which has high concentration as twice higher than other Gd-chelate. Thus, bolus injection of contrast media might induce strongly T2 shorting effects. Resultantly, less contrast enhancement in the pulmonary parenchyma could be expected. In the current study, simultaneous injection of Gadobutrol with slower injection rate of 1mL/sec and 2mL/sec injection rate of saline was made. This method might achieve dilution of the contrast media, and pulmonary parenchyma could be enhanced with good recognition, thus, pulmonary perfusion defect might be evaluated as minor fissures.Conclusion
Using fast imaging technique fat-sat DISCO with simultaneous bolus injection of Gadobutrol and saline, dynamic contrast MR imaging of the lung can steadily provide information of pulmonary vasculatures and perfusion of pulmonary parenchyma.Acknowledgements
No acknowledgement found.References
1) JMRI 2012; 35(6):1484Figures
Fig.1 Scores for overall image quality, homogeneity of signal intensity, and artifacts for blur and noise are demonstrated in the selected phase in the visualization of each structure. Each structure is well recognized except the right and left ventricles.
Fig.2 All segments of the pulmonary arteries were recognized with high confidence level.
Note: Main pulmonary A(MPA), Right & Left pulmonary A(R,L-PA), Right & Left branches Apical posterior(R,L-AP), Right Ascending(R-A), Right & Left Anterior(R,L-A), Right & Left Superior(R,L-S), Right & Left Descending(R,L-D), Right Middle lobe (R-ML), Right Basal Lateral(R-BL), Anterior(R-BA), Posterior(R-BP), Medial(R-BM), Left. Lingular Superior (L-SL), Inferior (L-IL), Left Basal Lateral (L-BL), Anteromedial (L-AM), Posterior (L-BP).
Fig.4 A: All pulmonary veins were well recognized. B: Inhomogeneity of parenchymal enhancement was noted provably due to sensitivity to the multi-coil and gravity.
Note: Right & Left superior, inferior pulmonary veins (R-S, R-I, L-S, L-I), Middle lobe V (W-M), Lingual V (L-V). Pulmonary parenchyma anterior, middle, posterior portions, Fat-sat M, Fat-sat SC.