0915
Lipid-insensitive 4D motion-resolved free breathing coronary MRA in heart transplant recipients at 3T1Department of Radiology, University Hospital (CHUV) and University of Lausanne (UNIL), Lausanne, Switzerland, 2School of Biomedical Engineering and Imaging Sciences, King’s College London, Lausanne, Switzerland, 3Cardiology Service, Lausanne University Hospital (CHUV), Lausanne, Switzerland, 4Advanced Clinical Imaging Technology, Siemens Healthcare AG, Lausanne, Switzerland, 5Center for Biomedical Imaging, Lausanne University Hospital (CHUV), Lausanne, Switzerland
Synopsis
The purpose of this study was to investigate coronary magnetic resonance angiography (MRA) at 3T as a possible alternative to invasive X-ray coronary angiography for the visualization of proximal and mid segments of the coronary arterial system in heart transplant recipients. Therefore, a lipid-insensitive binomial off-resonance excitation (LIBRE) pulse was optimized and combined with a 3D radial whole-heart sequence. Respiratory-self-navigated MRA was performed at 3T in heart transplant recipients during and after Gd infusion, and was compared with respiratory-motion compensation using compressed sensing (CS) to define the preferred acquisition and reconstruction protocol in this patient group.
Background
In heart transplant patients, there is a high prevalence of cardiac allograft vasculopathy (CAV), which is a major contributor to subsequent heart failure. Usually, CAV is detected on X-ray coronary angiography. The purpose of this study was to investigate coronary magnetic resonance angiography (MRA) at 3T as a possible alternative to invasive X-ray coronary angiography for the visualization of proximal and mid segments of the coronary arterial system. To this end, a lipid-insensitive binomial off-resonance excitation (LIBRE) pulse [1] was optimized and combined with a 3D radial whole heart sequence [2]. Respiratory-self-navigated MRA was performed at 3T in heart transplant recipients during and after Gd infusion, and was compared with respiratory motion compensation using compressed sensing (CS) to define the preferred acquisition and reconstruction protocol in this patient group.Materials and Methods
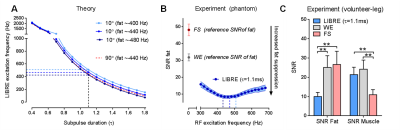
LIBRE optimization: To provide robust fat suppression, a LIBRE pulse was implemented and optimized for a pulse duration of 2τ=2.2ms through Bloch equation simulations as described in [1]. LIBRE fat suppression was measured in phantom and volunteer (legs) experiments, and compared with conventional fat suppression techniques (fat saturation (FS) and 1-180°-1 water excitation (WE)). Experiments were performed using a prototype 3D radial GRE acquisition with a segmented phyllotaxis trajectory [2], an isotropic voxel size (1.1mm3), and T2-preparation [3], on a clinical 3T MRI system (MAGNETOM Prisma, Siemens). Patient study: Cardiac allograft transplant patients (n=23) ≥6 months after transplantation were recruited and underwent their routine clinical exams as well as cardiac MR. Free-breathing ECG-triggered respiratory-self-navigated MRA [2] with LIBRE pulses was performed during and after gadolinium contrast agent injection [4, 5] with above described sequence (acquisition time ~8-10 min). Coronary X-ray angiograms were visually compared with MRA. Motion compensation: Each acquired segment was preceded by one readout oriented along the superior-inferior (SI) direction. To compensate for respiratory motion both the slow infusion and the late enhancement datasets were reconstructed with 1D self-navigation [2], a method that uses the SI image projection as motion reference [2], as well as with a respiratory-motion-resolved reconstruction that uses CS [6] and a previously presented automated self-gated (SG) method of the respiratory signal to resolve the data into 4 respiratory bins [7]. The respiratory phase with sharpest boundaries between the liver-lung interface was selected for data analysis, as assessed by visual inspection. Data analysis: Fat suppression using LIBRE was evaluated with a paired Student’s t-test on phantom and volunteer data. In patients, coronary vessel sharpness and length [8] was quantified in all acquired and reconstructed data (four 3D whole-heart datasets per patient). Two-way ANOVA with repeated measures was performed, with “contrast” and “motion-compensation method” as factorials, and followed by a two-tailed Student’s t-test for paired data as post-hoc test. p<0.05 was considered statistically significant.Results and Discussion
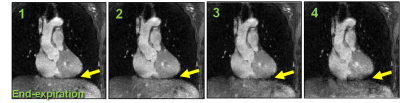
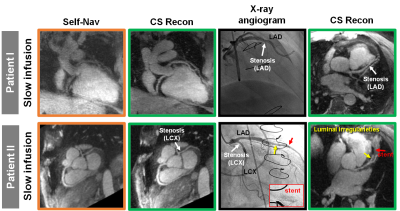
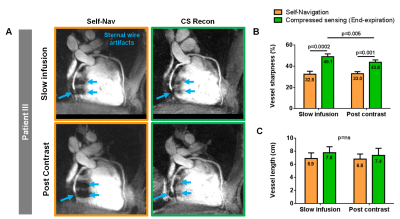
LIBRE optimization: Simulations showed that LIBRE provided robust nulling of the fat signal around a frequency of 470Hz, assuming a resonance frequency of fat at -440Hz (Fig. 1A). Phantom experiments showed a fat SNR decrease to 8.5±0.9 using LIBRE (with RF frequency of 480Hz) compared with 48.1±3.4 (FS) and 31.8±2.1 (WE) (Fig 1B). Volunteer experiments showed a decreased fat SNR of 9.9±2.2 using LIBRE compared with 25.1±6.1 (WE) and 26.6±6.9 (FS) (Fig. 1C). The decreased SNR in muscle tissue using the FS sequence can be mainly attributed to an increase in the noise in this 3D radial sequence (Fig. 1C). Patient study: The end-expiration phase typically showed the sharpest lung/liver interface (Fig. 2). Coronary reformats from MRA matched with irregularities observed on X-ray angiograms (Fig. 3). The second MRA (post-contrast) could not be acquired in 9/23 patients due to time constraints. Coronary reformats show improved data quality when CS was used (Fig. 4A). RCA vessel sharpness was significantly improved using CS, both during slow-infusion and post-contrast (From 32.5% to 49.1% and 33.0% till 43.8%, Fig. 4B). Vessel length measurements did not show significant differences across techniques (Fig. 4C). Respiratory-self-navigation performs a motion-correction along one dimension (superior-inferior direction), however, respiratory-motion-resolved reconstruction may simultaneously compensate for motion in multiple dimensions resulting in improved vessel conspicuity confirming the findings in [6]. Interestingly, when comparing the self-navigated reconstruction of the slow-infusion with post-contrast images, vessel sharpness did not significantly change. However, the motion-resolved reconstruction showed the highest average vessel sharpness in the slow-infusion images (49.1%, Fig. 4B).Conclusions
To the best of our knowledge, this is the first report of self-navigated whole heart imaging during and post slow Gd infusion in heart transplant recipients at 3T. Coronary artery visualization was significantly improved when CS was applied on data acquired during slow infusion.Acknowledgements
No acknowledgement found.References
[1] Bastiaansen JAM, Stuber M. Flexible water excitation. Flexible water excitation for fat-free MRI at 3 Tesla using lipid insensitive binomial off-resonant RF excitation (LIBRE) pulses. Magn Reson Med, In Press
[2] Piccini D, Littmann A, Nielles-Vallespin S, Zenge MO. Respiratory self-navigation for whole-heart bright-blood coronary MRI: methods for robust isolation and automatic segmentation of the blood pool. Magnetic resonance in medicine 2012;68(2):571-579.
[3] Nezafat R, Stuber M, Ouwerkerk R, Gharib AM, Desai MY, and Pettigrew RI. B1-Insensitive T2 Preparation for Improved Coronary Magnetic Resonance Angiography at 3 T. Magn Reson Med 2006; 55:858-864
[4] Liu X, Bi X, Huang J, Jerecic R, Carr J, Li D. Contrast-Enhanced Whole-Heart Coronary Magnetic Resonance Angiography at 3.0 T: Comparison With Steady-State Free Precession Technique at 1.5 T. Investigative Radiology. 43(9):663-668
[5] Yang Q, Li K, Liu X, Bi X, Liu Z, An J, Zhang A, Jerecic R, Li D. Contrast-Enhanced Whole-Heart Coronary Magnetic Resonance Angiography at 3.0-T: A Comparative Study With X-Ray Angiography in a Single Center. JACC 2009 54(1): 69-76
[6] Piccini D, Feng L, Bonanno G, Yerly J, Lim RP, Schwitter J, Sodickson D, Otazo R, Stuber M. Four-dimensional respiratory motion-resolved whole heart coronary MR angiography. MRM 2017; 77(4): 1473–1484
[7] Di Sopra, L., Piccini, D., Coppo, S., Bastiaansen, J., Stuber, M., and Yerly, J., Motion-Resolved 5D Imaging of the Heart: Time to Get Rid of the ECG?. In Proceedings of the 25th Annual Meeting of ISMRM, Honolulu, HI, USA, 2017, Program Number 3148
[8] Etienne A, Botnar RM, Van Muiswinkel AM, Boesiger P, Manning WJ, Stuber M. "Soap-Bubble" visualization and quantitative analysis of 3D coronary magnetic resonance angiograms. Magnetic resonance in medicine 2002;48(4):658-666.
Figures