0831
MRI predicts histopathologic composition of ileal Crohn's disease.1Radiology, Pitié Salpêtrière Hospital, UPMC, Paris, France, 2Translational and Molecular Imaging Institute, Icahn School of Medicine at Mount Sinai Hospital, New York, NY, United States, 3Pathology, Icahn School of Medicine at Mount Sinai Hospital, New York, NY, United States, 4Radiology, Icahn School of Medicine at Mount Sinai Hospital, New York, NY, United States, 5Gastroenterology, Icahn School of Medicine at Mount Sinai Hospital, New York, NY, United States
Synopsis
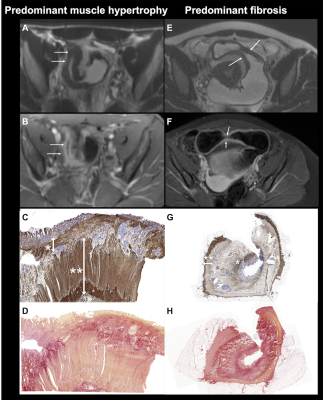
The aim of our study was to assess the value of MRI for the characterization of histopathologic tissue composition of small bowel Crohn’s disease (CD), including assessment of inflammation, fibrosis and smooth muscle hypertrophy. Our results showed that MRI-based parameters including ADC, MaRIA score and layered pattern of enhancement can predict the degree of bowel inflammation. We also showed that wall thickness measured on T2WI can distinguish prominent muscle hypertrophy from prominent fibrosis in ileal CD.
Introduction
Crohn’s disease (CD) is a chronic inflammatory bowel disease that can involve any location within the gastrointestinal tract but most frequently the distal small bowel (terminal ileum). Recently, smooth muscle hypertrophy has been suggested to be a contributor in small bowel lesions secondary to CD, in addition to inflammation and fibrosis (1). The aim of our study was to assess the value of MRI for the characterization of histopathologic tissue composition of small bowel CD, including inflammation, fibrosis and smooth muscle hypertrophy.Methods
35 consecutive patients (M/F 17/18, mean age 33y) with ileal CD who underwent small bowel resection (for stricture in 27 patients) and a preoperative contrast-enhanced MRI exam within one month before surgery were retrospectively included. Image assessment included qualitative parameters (pattern/degree of enhancement, presence of ulcerations/fistulas/abscesses), assessed by 2 radiologists in consensus and quantitative parameters [wall thickness on T2/T1WI, enhancement ratios, ADC, Clermont and MaRIA scores (as previously described] (2, 3). For ADC measurement and enhancement ration, free hand ROIs, including the largest part as possible of the involved segment were drawn by a 3rd observer. Inflammation was assessed by a semi-quantitative score. Immunostaining of smooth muscle actin (SMA) and Sirius red special stain for collagen deposition were performed to assess muscular hypertrophy and fibrosis. The ratio between normalized SMA and normalized Sirius red was calculated for all resected bowel segments. MRI parameters were compared with histopathologic findings including active inflammation, collagen deposition and muscle hypertrophy using Chi-2/Fisher or Mann-Whitney tests, and univariate/multivariate logistic/linear regression analyses.Results
Forty ileal segments were analyzed in 35 patients. Layered pattern at early-post-contrast phase was more prevalent (OR=8/p=0.015) ADC was significantly lower (OR=0.005/p=0.028) and MaRIA score was significantly higher (OR=1.125/p=0.013) in inflammation grades 2-3 compared to grade 1. Wall thickness on T2WI was significantly increased (OR=1.688/p=0.043), and fistulas (OR=14.5/p=0.017) were more prevalent in segments with disproportionately increased muscle hypertrophy vs. those with increased fibrosis. MaRIA/Clermont scores, wall thickness on T1WI and T2WI and ADC were all significantly correlated with degree of muscular hypertrophy, while no parameters correlated with degree of fibrosis. For identifying inflammation, MaRIA score had the best accuracy (AUROC 0.736, p=0.013) and for identifying prominent muscle hypertrophy, wall thickness on T2WI had the best accuracy (AUROC 0.742, p=0.028).Discussion
Our results showed that MRI can predict histopathologic composition of ileal CD including inflammation/edema and disproportionately increased muscular hypertrophy over fibrosis. The composition of ileal lesions is usually assessed with pathology on surgical specimen, but is important for treatment management. First, inflammation should be treated by medical therapy including anti-inflammatory treatment and not by surgery. Second, the presence of fibrosis and muscular hypertrophy can influence the treatment and surgical planning. Indeed, a stricture with prominent muscular hypertrophy will not likely respond to new antifibrotic agents than in those with excessive collagen deposition, and may be treated by surgery, while a stricture with prominent fibrosis may potentially benefit from new antifibrotic agents.Conclusion
MRI predicts the degree of inflammation, and can distinguish prominent muscle hypertrophy from prominent fibrosis in ileal CD with reasonable accuracy (AUROC>0.7).Acknowledgements
This work was partially supported by the Sanford J Grossman Charitable Trust for Integrative Studies in IBD, Société Française de Radiologie and NIH U01 DK62429, U01 DK062422, R01 DK092235.References
1. Chen W, Lu C, Hirota C, Iacucci M, Ghosh S, Gui X: Smooth Muscle Hyperplasia/Hypertrophy is the Most Prominent Histological Change in Crohn’s Fibrostenosing Bowel Strictures: A Semiquantitative Analysis by Using a Novel Histological Grading Scheme. J Crohns Colitis 2017; 11:92–104.
2. Hordonneau C, Buisson A, Scanzi J, et al.: Diffusion-weighted magnetic resonance imaging in ileocolonic Crohn’s disease: validation of quantitative index of activity. Am J Gastroenterol 2014; 109:89–98.
3. Rimola J, Rodriguez S, García-Bosch O, et al.: Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut 2009; 58:1113–1120.
Figures