0825
Differentiation of Mass-forming Focal Pancreatitis (MFFP) from Pancreatic Cancer (CP): Added Value of Magnetic Resonance Elastography (MRE) to Dynamic Contrast-enhanced Magnetic Resonance Imaging (DCE-MRI)1Shengjing Hospital of China Medical University, ShenYang, China, 2Philips Healthcare China, Beijing, China
Synopsis
The differential diagnosis of mass-forming focal pancreatitis (MFFP) and pancreatic cancer (PC) is clinically important. Our study shows that combined assessment of magnetic resonance elastography (MRE) with dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) is a promising technique with improved specificity of diagnosing PC from MFFP cases, when comparing with DCE-MRI.
Purpose
PC is one of the five most lethal malignancies worldwide. Currently, accurate differential diagnosis between MFFP and PC can guide clinical decision-making and avoid unnecessary pancreatectomy.1,2 Yet, this diagnosis is still challenging due to the significant overlap in radiological features based on current imaging modalities. DCE-MRI is one of the most important modality for detection, differentiation and staging PC. Recently, MRE showed that PC had significant higher stiffness than that of MFFP. 3 Herein, our study was to investigate if incorporating MRE with conventional DCE-MRI can provide a benefit in differentiating PC from MFFP.Methods
We retrospectively identified 15 MFFP and 27 PC patients confirmed by histopathologic examinations from Jan 2017 to Aug 2017. Only the patients with both valid DCE-MRI and MRE results were included. A radiologist with 20 year experience of abdominal imaging blindly reviewed all the images on DCE-MRI and determined the presence of pancreatic malignancy using a five-point confidence scale: 1=definitely malignant, 2=probably malignant, 3= equivocal lesion, 4=probably benign, 5=definitely benign. Sensitivity for diagnosing PC was determined by the number of patients with a score of 1 or 2. Diagnostic accuracy of DCE-MRI alone, and the combination of DCE-MRI with MRE was calculated using receiver operating characteristic (ROC) analysis. The combination of MRE (>2.38 kPa for malignancy determined by ROC analysis) and DCE-MRI was determined by a logistic regression analysis for calculating the probabilities. DCE-MRI was a conventional clinical scan sequence, performed with 3.0T scanner (Philips 3.0T Ingenia, Philips Healthcare, the Netherlands). MRE examinations were performed on another 3.0T MR scanner (Signa HDX 3.0T system; GE Healthcare, Milwaukee).The imaging parameters were as follows: frequency=40Hz; TR/TE = 1375/38.8ms; phase offsets = 3; FOV = 40 cm; matrix = 96×96; number of signal averages = 1; frequency-encoding direction = RL; parallel imaging acceleration factor = 3; number of slices = 32; thickness = 3.5mm.Results
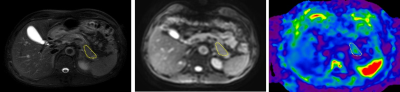
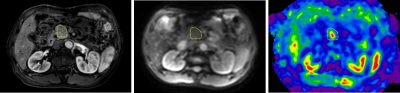
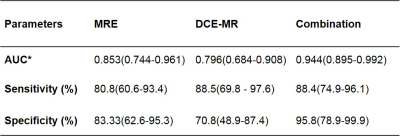
Figure 1 and 2 showed 2 cases with MFFP and PC masses as examples, respectively. PC showed higher stiffness (median [IQR], 3.21[2.43-3.72] kPa) than that of MFFP (2.01[1.72-2.32] kPa). DCE-MRI for differentiating PDAC from MFFP had an AUC of 0.796, with sensitivity of 88.5% and specificity of 70.8%. When both MRE and DCE-MRI were taken into account, the AUC (0.944) improved significantly than the result of DCE-MRI alone (P< 0.001), and specificity also increased significantly when compared with that of DCE-MRI alone (95.8% vs 70.8%, P= 0.03). The sensitivity was maintained (88.5 % vs 88.4 %, P=1.00) (Table 1).Discussion
In our study, the stiffness of PC was much higher than the stiffness of MFFP. Pathologically, PC has obvious fibrous tissue infiltrating and enveloping neoplasms, showing much higher stiffness than both MFFP. The widely-adopted DCE-MRI showed malignancy based on morphological imaging findings, such as indistinct margin of a solid mass, hypo-intensity on T1WI and hyper-intensity on T2WI, hypo-enhancement, obstruction of pancreatic duct and metastatic lesions, etc. The combination of DCE-MRI and MRE, indicating both morphological and mechanical changes, offered both high specificity (95.8%) and sensitivity (88.5%). This indicates that MRE had an added value for improved specificity to help DCE-MRI to diagnose MFFP from being misdiagnosed as malignancy.Conclusion
Combined assessment using the noninvasive imaging methods - MRE and DCE MRI -improves specificity of diagnosing PC from MFFP cases, and it is promising for clinical uses.Acknowledgements
We thank Richard Ehman and Kevin Glaser from the Mayo Clinic for providing the MRE system, Jun Chen from the Mayo Clinic for his assistance with providing the tailored pancreatic MRE driver.References
1. Hur BY, Lee JM, Lee JE et al (2012) Magnetic resonance imagingfindings of the mass‐forming type of autoimmune pancreatitis:Comparison with pancreatic adenocarcinoma. J Magn ResonImaging 36:188–197
2. Sugiyama Y, Fujinaga Y, Kadoya M et al (2012) Characteristicmagnetic resonance features of focal autoimmune pancreatitis usefulfor differentiation from pancreatic cancer. Jpn J Radiol 30:296–309
3. Shi Y, Gao F, Li Y et al (2017) Differentiation of benign and malignant solid pancreatic masses using magnetic resonance elastography with spin-echo echo planar imaging and three-dimensional inversion reconstruction: a prospective study. Eur Radiol. 10.1007/s00330-017-5062-y
Figures