0820
Magnetic resonance measurements of fat content and water diffusion in muscles of glucocorticoid-treated patients with polymyalgia rheumatica compared with healthy volunteers.1NIHR Musculoskeletal Biomedical Research Centre, Leeds, United Kingdom, 2Leeds Institute of Rheumatic and Musculoskeletal Medicine, Leeds, United Kingdom, 3Siemens Healthcare GmbH, Erlangen, Germany, 4School of Human and Health Science, University of Huddersfield, Huddersfield, United Kingdom, 5School of Medicine, University of Leeds, Leeds, United Kingdom
Synopsis
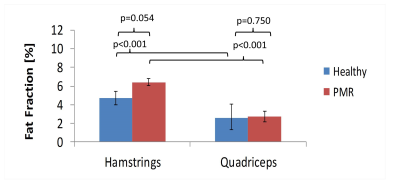
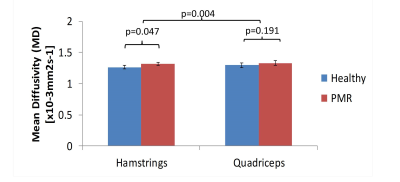
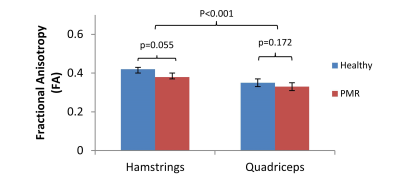
The purpose of this study was to assess differences in fat fraction and water diffusion between muscles in the healthy thigh and to assess differences between glucocorticoid treated patients with polymyalgia rheumatic (PMR) and healthy controls. Twenty five healthy volunteers and sixteen patients with PMR undergoing glucocorticoid treatment underwent MRI to assess muscle fat fraction and diffusion. The study found that the hamstrings have greater fat fraction and reduced diffusion compared to quadriceps in healthy individuals. Furthermore, alterations in fat fraction and diffusion parameters associated with glucocorticoid-treated PMR are more readily detectable in the hamstrings than the quadriceps.
Introduction
Polymyalgia rheumatica (PMR) is an inflammatory disease causing pain, stiffness and impairment of function of the muscles. The mainstay of treatment is systemic glucocorticoid (GC) therapy which may itself cause myopathy 1. Thus both PMR and glucocorticoids have the potential to adversely affect muscle structure and function creating a need for more sensitive markers of muscle change in response to PMR and GC treatment. MR measurements of fat fraction and diffusion have shown promise in characterising muscle and monitoring muscle disease 2–6. MR fat fraction measurements are sensitive to muscle changes due to idiopathic inflammatory myopathies 5 and sarcopenia 6, and water diffusion measurements are sensitive to changes in muscle tissue microstructure due to muscle pathology 6–9. The objectives of this study were to determine whether MR can detect differences in fat fraction and water diffusion measurements; firstly, between muscle groups in the healthy thigh, and secondly, between muscle groups of GC-treated patients with PMR compared to healthy volunteers.Methods
25 healthy volunteers (mean age 38 years 15/25 males) and 16 patients with PMR undergoing glucocorticoid treatment (mean age 69 years, 2/16 males) were included in this NREC ethically approved prospective pilot study. Magnetic resonance images of the mid-thigh were acquired using a MAGNETOM Verio 3T MR scanner (Siemens Healthcare). Fat fraction was assessed using a 2-point VIBE Dixon volume: 200 x 300 x 300 mm3, 40 slices, 5 mm thickness, TR 11ms TE 2.45 ms & 3.675 ms, flip angle 15o. Diffusion imaging was performed using a stimulated acquisition mode (STEAM) prototype sequence with an echo planar imaging (EPI) readout using spectral attenuated inversion recovery (SPAIR) fat suppression: FOV: 300 x 300 mm, TR/TE: 6300/42.4 ms, slice thickness 5 mm, matrix 128x128, nominal b-values of 0 and 500 mm2s-1, 6 diffusion directions and an echo spacing of 0.76 ms. A long diffusion mixing time of 980 ms was used to maximise sensitivity to restricted diffusion in the relatively large diameter muscle fibres. Mean diffusivity (MD), fractional anisotropy (FA) and eigenvalue (λ1-3) parameter maps were generated. Regions of interest were drawn around each of the individual muscles that make up the hamstrings and quadriceps to generate an overall mean value for each of these two muscle groups (figure 1). A linear mixed model was used to test for differences between muscle groups and for differences between patients and healthy volunteers, accounting for differences in age and gender between groups. All results are presented as (mean (95% confidence interval); p-value) unless otherwise stated.Results
Comparing hamstrings and quadriceps, significant differences were observed in both fat fraction and diffusion indices (figures 2-4). Fat fraction was approximately twice as high in the hamstrings relative to the quadriceps in both the healthy (ratio quadriceps:hamstrings 0.55 (0.49, 0.61); p<0.001) and patient (0.42 (0.37, 0.49); p<0.001) groups. In the diffusion measurements, the hamstrings exhibited a lower mean adjusted difference in MD (0.02 (0.01, 0.04); p=0.004), λ2 (0.08 (0.06, 0.10); p<0.001); λ3 (0.06 (0.05, 0.08); p<0.001) and higher FA (-0.06 (-0.07, -0.05); p<0.001) and λ1 (0.07 (-0.09, -0.05); p<0.001) than the quadriceps. Comparing patients and healthy volunteers, there was no difference in fat fraction or diffusion between patients and the healthy group in the quadriceps (figures 2-4). However, there were small, borderline significant differences in the hamstrings, with a higher fat fraction [ratio patients : volunteers 1.37 (0.99, 1.87), p=0.054], increased MD [0.05 (0.0, 0.1), p=0.05], λ2 0.09 (0.01, 0.16), p=0.019); λ3 (0.06 (0.00, 0.13), p=0.064) and reduced FA -0.03 (-0.07, 0.00); p=0.055 (values are mean adjusted differences). The difference in fat fraction between the patient and healthy groups was greater in the hamstrings than in the quadriceps with (p=0.005).Conclusion
This study demonstrates significant differences in fat and diffusion measurements between the quadriceps and hamstrings muscles, with the hamstrings exhibiting higher fat content and reduced mean diffusion. Differences between patients and healthy controls were negligible in the quadriceps but approached significance in the hamstrings. The difference in fat fraction between the patient and control groups was significantly higher in the hamstrings than in the quadriceps, implying that changes in muscle fat in glucocorticoid-treated patients with PMR are more readily detectable in the hamstrings than in the quadriceps.Acknowledgements
JDB is funded by a National Institute for Health Research (and Health Education England, Clinical Lectureship. This paper presents independent research funded by the National Institute for Health Research (NIHR) and Health Education England. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. SLM was supported by a Clinician Scientist Award from the National Institute for Health Research (NIHR). Recruitment and imaging of patients with polymyalgia rheumatica (STAY-ACTIV) was supported by a EU grant to Professor Paul Stewart, PRECORT. The research is supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre. We are grateful to Rob Evans and Brian Chaka for carrying out the MR studies.References
1. Gupta A, Gupta Y. Glucocorticoid induced myopathy: Pathophysiology, diagnosis, and treatment. Indian J Endocrinol Med. 2013;17(5):913–6.
2. Li K, Dortch RD, Welch EB, et al. Multi-parametric MRI characterization of healthy human thigh muscles at 3.0 T - relaxation, magnetization transfer, fat/water, and diffusion tensor imaging. NMR Biomed. 2014;27(9):1070–84.
3. Kumar D, Karampinos DC. Quadriceps intramuscular fat fraction rather than muscle size is associated with knee osteoarthritis. Osteoarthr Cartil. 2014;22(2):226–34.
4. Triplett WT, Baligand C, Forbes SC, et al. Chemical shift-based MRI to measure fat fractions in dystrophic skeletal muscle. Magn Reson Med. 2014;72:8–19.
5. Yao L, Yip AL, Shrader JA, et al. Magnetic resonance measurement of muscle T2, fat-corrected T2 and fat fraction in the assessment of idiopathic inflammatory myopathies. Rheumatology. 2016;55:441–9.
6. Melville DM, Mohler J, Fain M, et al. Multi-parametric MR imaging of quadriceps musculature in the setting of clinical frailty syndrome. Skeletal Radiol. 2016;45(5):583–9.
7. Scheel M, von Roth P, Winkler T, et al. Fiber type characterization in skeletal muscle by diffusion tensor imaging. NMR Biomed. 2013;26(10):1220–4.
8. Qi J, Olsen NJ, Price RR, et al. Diffusion-weighted imaging of inflammatory myopathies: Polymyositis and dermatomyositis. J Magn Reson Imaging. 2008;27(1):212–7.
9. Sigmund EE, Sui D, Ukpebor O, et al. Stimulated echo diffusion tensor imaging and SPAIR T2 -weighted imaging in chronic exertional compartment syndrome of the lower leg muscles. J Magn Reson Imaging. 2013;38(5):1073–82.
Figures