0768
Myocardial Edema Imaging – A Comparison of Three Techniques1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, China, 2Department of Medicine (Cardiovascular Division), Beth Israel Deaconess Medical Center and Harvard Medical School, Boston, MA, United States, 3Department of Cardiology, West China Hospital, Chengdu, China, 4Siemens Healthcare Pte Ltd., Singapore, Singapore
Synopsis
Myocardial edema is commonly imaged using T2 based imaging technique, such as T2w-TSE, T2p-bSSFP and T2 mapping. Noting its elevated T1 and T2 value, a single-shot technique using T2 prepared STIR called T2STIR-bSSFP has been proposed for edema imaging. This study compared the contrast of T2p-bSSFP, T2 mapping and the newly proposed T2STIR-bSSFP methods via simulation, phantom experiment and patient study. The results showed that T2STIR-bSSFP has the highest contrast in myocardial edema image among the three methods at a shot scan time. It may provide a fast edema imaging technique for the whole heart covering.
INTRODUCTION
Myocardial edema in acute myocardial infarction (AMI) is commonly imaged using dark blood T2w-TSE [1]. However, its sensitivity to cardiac motion may result in signal inhomogeneity in the images. Single-shot T2-prepared bSSFP (T2p-bSSFP) overcomes these issues and was found superior to T2w-TSE [2]. T2 mapping proposed later allows T2 quantification of myocardium [3]. Noting that both T1 and T2 are elevated in edema, a single-shot technique using T2 prepared STIR (short tau inversion recovery), called T2STIR-bSSFP, has been proposed for edema imaging [4]. This study compares the contrast between edema and remote myocardium for the three gradient echo based sequences via simulation, phantom experiment and patient study.METHODS
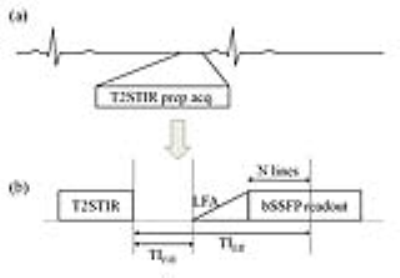
Figure 1 shows the T2STIR-bSSFP sequence.
Simulation: Bloch equation simulation was performed using MATLAB (MathWorks, USA). The signal difference and contrast ratio between normal and edematous myocardium in T2p-bSSFP and T2STIR-bSSFP were compared. The echo time (TEprep) in T2STIR and T2 preparation modules was varied from 40-70ms. Parameters for bSSFP readout were: 10 LFA pulses, 22 phase encoding lines before the k-space center, flip angle=60o, TE/TR=1.45/2.9ms. T1/T2 values for normal and edematous myocardium were 1147ms/51ms and 1454ms/75ms respectively (MR relaxation parameters of the phantom). For T2 mapping, T2 values were taken as signals.
Phantom experiment: It was performed on a 3T clinical system (TIM TRIO, Siemens). The phantom had two compartments: edematous and normal myocardium, built with agar doped with NiCl2. The compartments’ T1 and T2 values were measured with an inversion recovery spin echo and a spin echo sequence respectively. See above for their T1 and T2 values. The phantom was imaged with T2p-bSSFP, T2 mapping and T2STIR-bSSFP triggered with pseudo ECG (RR interval=800ms). For T2p-bSSFP and T2STIR-bSSFP, TEprep was varied from 40-70ms. Images were reconstructed in identical way. Imaging parameters were: pixel size=1.6ⅹ1.6mm2, thickness=8mm, TE/TR=1.45/2.9ms, flip angle=60o. The experiments were repeated four times. Results were averaged. Dependence of contrast to noise ratio (CNR) and contrast ratio between the two phantom compartments on TEprep for T2p-bSSFP and T2STIR-bSSFP were found. In T2 mapping, the contrast ratio, given by the ratio between the T2 values of the two compartments, was independent of TEprep.
Patient study: The ability of T2p-bSSFP, T2 mapping and T2STIR-bSSFP in detecting edema was evaluated in patients. The study was IRB approved. Six patients with acute myocardial infarction and one patient with radiofrequency ablation induced infarct/edema were recruited. Informed consents were obtained. Each patient was imaged with the three sequences. As part of the clinical protocol, the patient was also imaged with T2w--TSE, T1 mapping pre-contrast, and finally Late Gadolinium Enhancement (LGE) post-contrast, i.e, ~10 minutes after contrast agent (Magnevist, 0.15mmol/kg) injection. See Table 1 for the imaging parameters used.
RESULTS AND DISCUSSION
Figure 2 shows the results from simulation and how they compared to the phantom experiment. Phantom results matched simulation very well. T2STIR-bSSFP gave higher contrast ratio and signal difference than other sequences despite its short scan time.
In patients, the CNR and contrast ratios from the sequences also showed that T2STIR-bSSFP outperformed other techniques (Figure 3). Figure 4 shows one patient case. The high signal corresponds to edema and was well depicted from normal myocardium (its signal was suppressed). Robust fat suppression in T2STIR images, unavailable in other techniques, allows for better delineation of myocardium from its surrounding tissues. Clinically, this unique feature would also help distinguish between fat and any effusion around the heart.
Previous studies showed that T2p-bSSFP is more robust than T2w-TSE in myocardial edema imaging [5]. T2 mapping essentially extends T2p-bSSFP. Both techniques exploited only T2 changes in edema. T2STIR-bSSFP improves edema-myocardium contrast by augmenting the T2 elevation with T1 elevation unique in edema. Though STIR-bSSFP cannot quantify T1 and T2 of edematous myocardium, the single-shot technique can “scout” for edema in the whole heart without breathholding in CMR examinations. Breathholding T1 and T2 mapping examinations can then be used to quantify the edematous regions so identified. The technique will be a very useful addition to the CMR toolbox.
CONCLUSION
Among the three techniques, T2STIR-bSSFP has the highest contrast in myocardial edema imaging while having the shortest scan time. T2STIR-bSSFP may greatly shorten the scan time for identifying myocardial edema over the whole heart.Acknowledgements
National Natural Science Foundation of China (No. 61401449, 6177012328 ).References
[1]. Simonetti OP, Finn JP, White RD,et.al., "Black blood" T2-weighted inversion-recovery MR imaging of the heart. Radiology 1996;199(1):49-57.
[2]. Kellman P, Aletras AH, Mancini C, et.al., T2-prepared SSFP improves diagnostic confidence in edema imaging in acute myocardial infarction compared to turbo spin echo. Magn Reson Med 2007;57(5):891-897.
[3].Giri S, Chung YC, Merchant A, et.al., T2 quantification for improved detection of myocardial edema. J Cardiovasc Magn Reson 2009, 11:56.
[4].Yanjie Zhu, Dan Yang, Yucheng Chen, et.al., Myocardial Edema Imaging using Single-shot T2STIR Prepared bSSFP, ISMRM 2017, p3252
[5]. Alexander R. Payne, Colin Berry, Peter Kellman, et.at., Bright Blood T2-Weighted MRI Has High Diagnostic Accuracy for Myocardial Hemorrhage in Myocardial Infarction: A Preclinical Validation Study in Swine, Circ Cardiovasc Imaging, 2011, 4(6):738-745
Figures