0763
Pericardial Enhancement in Recurrent and Constrictive Pericarditis: Correlation with Pathology in 52 PatientsJames Glockner1
1Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Pericardial late gadolinium enhancement was correlated with pathologic specimens in 52 patients who had pericardiectomy performed for constrictive or chronic pericarditis. Pericardial LGE is an indicator of pericardial inflammation; however, it does not reliably distinguish inflammation from fibrosis: LGE was seen in 9/10 patients with pericardial fibrosis and minimal or no pericardial inflammation. Pericardial edema or early pericardial enhancement may be more useful biomarkers for pericardial inflammation.
Introduction
Pericardial late gadolinium enhancement (LGE) has been correlated with pathologic evidence of inflammation, and therefore cardiac MRI may be useful in assessing the extent of pericardial inflammation as well as in evaluating the response of patients with pericarditis to anti-inflammatory medical therapy. Fibrotic pericardial thickening in the setting of chronic or recurrent pericarditis may also demonstrate enhancement, however, and this may limit the utility of LGE images in quantifying active inflammation. We evaluated cardiac MRI examinations in 52 patients who had subsequent pericardiectomy for constrictive or chronic pericarditis to assess how well the presence and extent of pericardial enhancement on LGE images correlated with the presence of inflammation at pathology.Materials and Methods
A search of the cardiac MRI database revealed 52 patients who had MRI performed between 2014 and 2017 for indications including pericarditis and had subsequent cardiac surgery which included partial or complete pericardiectomy or pericardial biopsy performed within 6 months of the MRI. LGE images were assessed for the presence or absence of pericardial enhancement, and when present was quantified as mild, moderate, or severe. Early post-gadolinium images (acquired 1 – 3 minutes following gadolinium injection) were also assessed when present. Triple inversion recovery T2-weighted images were also assessed for the presence or absence of pericardial edema.Results
Pathologic specimens were involved by both fibrous thickening and predominantly lymphocytic infiltration in a majority of specimens (42). In these patients, pericardial LGE was noted in 40/42 cases. In 10 patients, an inflammatory component was either absent or described as minimal. Pericardial LGE was present in 9/10 of these patients, classified as mild in 6 and moderate in 3 (Fig. 1). Mild pericardial edema was noted in 2 of these patients, and early pericardial enhancement in none of these patients (with early enhancement images available in 5/10). Pericardial inflammation was graded as moderate in 11 patients and marked in a single patient. Pericardial LGE was present in all of these patients, classified as moderate or marked in 7 and mild in 4. Pericardial edema was present in 7 patients, and early pericardial enhancement was seen in 3 of 4 patients with available data.Discussion
Although pericardiectomy remains the gold standard therapy for constrictive pericarditis, the not insignificant associated morbidity and mortality have led some cardiologists to advocate a trial of anti-inflammatory medication in patients who are not severely symptomatic. Cardiac MRI can potentially be used to assess the presence and extent of pericardial inflammation at baseline, thereby identifying patients most likely to respond to anti-inflammatory therapy, and can also evaluate response to therapy. Pericardial LGE is a reliable indicator of pericardial inflammation; however, in the setting of constrictive pericarditis or chronic pericarditis, the presence of pericardial fibrosis can be a confounding variable – we saw LGE in 9/10 patients who had no or minimal inflammation in their pathologic specimens. Pericardial edema and early pericardial enhancement had better correlation with pathologic inflammation, and these may be more useful biomarkers of pericardial inflammation.Acknowledgements
No acknowledgement found.References
No reference found.Figures
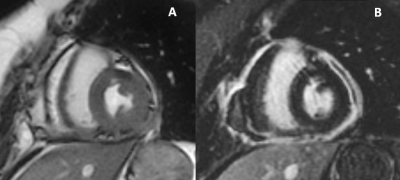
Patient with
constrictive pericarditis with minimal lymphoplasmacytic infiltrate and marked
non-calcific fibrous thickening of the pericardiectomy specimen. Short axis b-SSFP image (A) demonstrates
moderate diffuse pericardial thickening.
Short axis LGE image (B) shows moderate – marked diffuse pericardial
enhancement.