0762
Myocardial T1 And T2 Mapping Using MR Fingerprinting: Comparison to clinical standards1Radiology, University Hospitals Cleveland Medical Center, Cleveland, OH, United States, 2Biomedical Engineering, Case Western Reserve University, Cleveland, OH, United States, 3Case Western Reserve University, Cleveland, OH, United States, 4Case Western Reserve University School of Medicine, Cleveland, OH, United States, 5Case Western Reserve University School of Medcine, Cleveland, OH, United States, 6Cardiology, University Hospitals Cleveland Medical Center, Cleveland, OH, United States
Synopsis
Myocardial T1 and T2 relaxation times obtained with MRF were compared to values from traditional mapping sequences (MOLLI and T2-prep bSSFP) and evaluated for repeatability and reproducibility in 50 normal volunteers, as per SCMR consensus guidelines. MRF compared favorably with traditional sequences without significant proportional or systemic differences with fair to excellent repeatability and reproducibility, while providing better image quality.
Introduction
Traditional cardiac tissue property mapping1,2 techniques are prone to errors due to deviation of collected signals from the relaxation model, respiratory motion and heart rate variations. Cardiac MR Fingerprinting (cMRF) allows simultaneous mapping of multiple tissue properties, and because the cMRF dictionary incorporates heart rate variations into the signal model, cMRF may result in fewer artifacts and more accurate quantitative values3,4. The goal of this work was to: a) compare MRF-derived T1 and T2 relaxation times with those from modified Look-Locker inversion recovery (MOLLI) and T2-prepared balanced steady-state free precession (bSSFP) techniques in normal volunteers; b) evaluate same day repeatability, intra- and inter-reader reproducibility, and image quality of these techniques.Methods
T1 and T2 maps were acquired in three short axis slices in 50 healthy volunteers (M:F 27:23; average heart rate 73 bpm) at 1.5 T (Siemens Aera) using a cMRF sequence with ECG triggering in diastole and a breathhold duration of 15 heartbeats (192x192 matrix, 300mm2, 1.6x1.6x8.0mm3 spatial resolution, TR 5.1ms, FA 4-25deg). Standard T1 maps were acquired using MOLLI with 5(3)3 acquisition pattern, and standard T2 maps using a T2-prep bSSFP sequence with preparation times of 0, 25, and 55ms5,6. Repeatability was tested for all sequences by acquiring a mid-ventricular slice at the beginning and end of scan session. cMRF data were processed in MATLAB to generate T1 and T2 maps; regions of interest (ROIs) were drawn across 16 standardized AHA segments on MRF, MOLLI and bSSFP derived T1 and T2 maps (segment 17 was excluded due to poor image quality in all cases). Mean relaxation times were obtained at segment and slice levels. To test intra- and inter-reader reproducibility, ROIs were drawn on the mid-ventricular slice by two raters in 20 randomly selected datasets on all sequences.
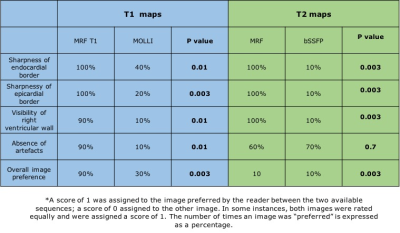
Image quality comparisons were performed between the techniques in 10 randomly selected datasets by a blinded cardiologist. The following criteria were used to evaluate image quality: a) sharpness of endocardial border; b) sharpness of epicardial border; c) visibility of right ventricular wall; d) absence of artefacts; e) overall image preference (Figure 5). A binary scale was used by the rater to compare MRF-derived T1 and T2 maps with MOLLI and bSSFP derived maps. A score of 1 was assigned to the preferred image and 0 to the less preferred image; both images were assigned a score of 1 if they were equally preferable.
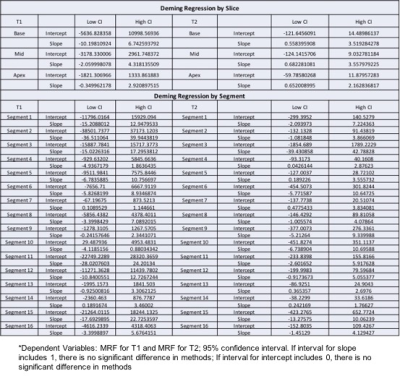
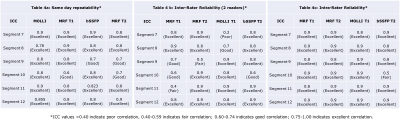
Deming regression analysis was used to compare proportional and systematic errors between the sequences. Repeatability, intra- and inter-reader reproducibility were assessed using intra-class coefficient (ICC). McNemar test was applied to evaluate if there was a statistically significant difference in the number of times one sequence was preferred over the other for each criterion. Statistical analysis was performed using SPSS (IBM, IL, version 22.0).
Results
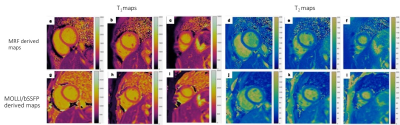
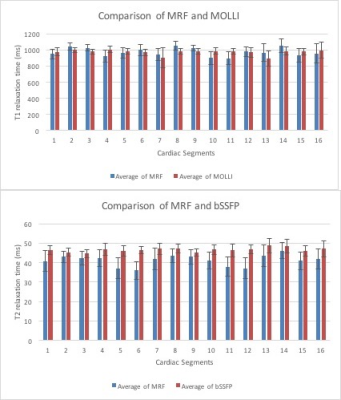
The average myocardial T1 relaxation time was 964.4±71.8 ms with cMRF, 978.8± 33.7 ms with MOLLI; average T2 relaxation time was 41.2±4.2 ms with cMRF, 46.6±2.7ms with bSSFP (Figure 1, 2). Deming regression analysis revealed no proportional or systematic errors between the methods except for segment 10(Figure 3). ICC revealed fair to excellent repeatability for same day measurements for all sequences (Figure 4a), as well as for intra- (Figure 4b) and inter-reader reproducibility (Figure 4c). MRF-derived maps were preferred over traditional sequences for both T1 and T2 maps with p-values ≤ 0.01 (Figure 5).Discussion
Studies have shown that myocardial T1 values could have prognostic value in diastolic dysfunction, cardiomyopathy of varying etiology, heart failure and infiltrative disorders of the myocardium7-10. As per the SCMR consensus statement, a mapping technique should be benchmarked against previously reported myocardial relaxometry values and local normative values established for application on a patient population11. A normative dataset of at least 50 subjects is required for diseases with low magnitude biological change11. No proportional or systematic differences were found in the relaxometry values provided by MRF and traditional methods in our study of 50 healthy subjects; the difference in segment 10 could be related to chance in this dataset of 3200 segment-level measurements. The standard deviation for MRF-derived values was larger than that for commercially available sequences, potentially due to application of filters on commercial mapping methods that reduce the observed variation in an ROI. However, the image quality comparison by a blinded reader revealed that MRF-derived maps were preferred over traditional sequences. MRF also compared favorably with traditional methods in repeatability and reproducibility measures while yielding simultaneous T1 and T2 maps.Conclusion
MRF provides repeatable and reproducible cardiac relaxometry values with better image quality compared to traditional mapping approaches.Acknowledgements
This work is funded by NIH/NHLBI grants: 2R01HL094557, 1R01DK098503 and 1R01EB016728, and Siemens Healthineers.References
1. Hamlin SA, Henry TS, Little BP, Lerakis S, Stillman AE. Mapping the future of cardiac MR imaging: case-based review of T1 and T2 mapping techniques. Radiographics. 2014;34(6):1594-611. Epub 2014/10/14. doi: 10.1148/rg.346140030. PubMed PMID: 25310419.
2. Kellman P, Hansen MS. T1-mapping in the heart: accuracy and precision. J Cardiovasc Magn Reson. 2014;16:2. Epub 2014/01/07. doi: 10.1186/1532-429x-16-2. PubMed PMID: 24387626; PubMed Central PMCID: PMCPMC3927683.
3. Ma D, Gulani V, Seiberlich N, Liu K, Sunshine JL, Duerk JL, et al. Magnetic resonance fingerprinting. Nature. 2013;495(7440):187-92. Epub 2013/03/15. doi: 10.1038/nature11971. PubMed PMID: 23486058; PubMed Central PMCID: PMCPMC3602925.
4. Hamilton JI, UniversityCleveland BEWR, Jiang Y, UniversityCleveland BEWR, Chen Y, yxc235@case.edu, et al. MR fingerprinting for rapid quantification of myocardial T1, T2, and proton spin density. Magnetic Resonance in Medicine. 2017. doi: 10.1002/mrm.26216.
5. Messroghli DR, Radjenovic A, Kozerke S, Higgins DM, Sivananthan MU, Ridgway JP. Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med. 2004;52(1):141-6. Epub 2004/07/06. doi: 10.1002/mrm.20110. PubMed PMID: 15236377.
6. Piechnik SK, Ferreira VM, Dall'Armellina E, Cochlin LE, Greiser A, Neubauer S, et al. Shortened Modified Look-Locker Inversion recovery (ShMOLLI) for clinical myocardial T1-mapping at 1.5 and 3 T within a 9 heartbeat breathhold. J Cardiovasc Magn Reson. 2010;12:69. Epub 2010/11/26. doi: 10.1186/1532-429x-12-69. PubMed PMID: 21092095; PubMed Central PMCID: PMCPMC3001433.
7. Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S, et al. T1-Mapping and Outcome in Nonischemic Cardiomyopathy: All-Cause Mortality and Heart Failure. JACC Cardiovasc Imaging. 2016;9(1):40-50. Epub 2016/01/15. doi: 10.1016/j.jcmg.2015.12.001. PubMed PMID: 26762873.
8. Baksi AJ, Pennell DJ. T1 Mapping in Heart Failure. 2013. doi: 10.1161/CIRCIMAGING.113.001178.
9. Cardiac Imaging to Evaluate Left Ventricular Diastolic Function - ScienceDirect. 2017. doi: 10.1016/j.jcmg.2015.07.004.
10. Pontnau F, Kachenoura N, Bollache E, Soulat G, Ashrafpoor G, Perdrix L, et al. Associations between native myocardial T1 and diastolic function evaluated by PC-CMR in patients with severe aortic valve stenosis. Journal of Cardiovascular Magnetic Resonance. 2015;17(1). doi: 10.1186/1532-429X-17-S1-Q18.
11. Messroghli DR, Moon JC, Ferreira VM, Grosse-Wortmann L, He T, Kellman P, et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2* and extracellular volume: A consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). Journal of Cardiovascular Magnetic Resonance. 2017;19(1):75. doi: 10.1186/s12968-017-0389-8.
Figures