0720
Patient-Specific 3D Printed and Augmented Reality Prostate Cancer Models Derived from MRI Data: Initial Results from Prospective Clinical Study1Center for Advanced Imaging Innovation and Research (CAI2R) and Bernard and Irene Schwartz Center for Biomedical Imaging, Department of Radiology, NYU School of Medicine, New York, NY, United States, 2Division of Urologic Oncology, Department of Urology, NYU School of Medicine, New York, NY, United States
Synopsis
The objective of this study was to determine whether patient-specific 3D printed and augmented reality prostate cancer models derived from multi-parametric MRI data can influence pre-surgical planning and patient outcomes for patients undergoing robotic assisted radical prostatectomy. Initial results from our prospective study are presented.
Introduction
Patient-specific three-dimensional (3D) printed and augmented reality (AR) prostate cancer models can be derived from multi-parametric MRI data; and these models may help to provide surgeons with precise knowledge of the 3D location of the dominant tumor and its proximity to surrounding anatomical structures (1, 2). Although 3D models (either printed or AR) may provide better spatial orientation over conventional imaging for pre-operative planning, there is currently a paucity of data showing how such models may impact patient care. The objective of this study was to assess whether 3D printed and AR prostate cancer models can influence pre-surgical planning decisions as well as surgical metrics such as blood loss and operating times in patients undergoing robotic assisted prostatectomy.Methods
Patients with MRI-visible prostate cancer (PI-RADS v2 score ≥3) undergoing robotic assisted radical prostatectomy (from March 2017 – October 2017) were prospectively enrolled in this IRB approved study (n=42). Patients were randomized to one of three methods of pre-operative image data visualization by the operating surgeon: 1) imaging alone, 2) imaging plus a 3D printed model, or 3) imaging plus an AR model. 3D models were created from multi-parametric MRI data including T2WI, DWI, ADC, and DCE imaging. The dominant tumor, prostatic capsule, prostatic urethra, rectal wall, bladder neck, and neurovascular bundles were segmented and either 3D printed or viewed in an AR device (Figure 1). Surgeons with at least five advanced visualization cases were included in the evaluation. These surgeons completed a pre-operative survey (Figure 2) for all patients with imaging alone. For patients randomized to receive 3D printed or AR models, the survey was completed again after reviewing the model and survey results were compared to each other. Blood loss and operating times were measured and compared between groups using an unpaired t-test.Results
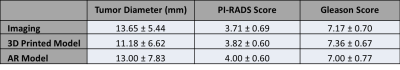
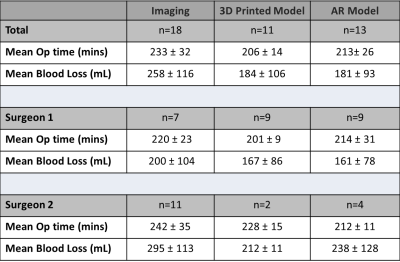
Out of 42 patients, there were 18 with imaging only, 11 with 3D printed models, and 13 with AR models. There were no significant differences in tumor size, PI-RADS score, or Gleason score between groups (Figure 3). By visual inspection, pertinent anatomical structures were well visualized for 10/11 of the 3D printed models and 12/13 AR models. One surgeon reported that the apical extent of the prostate was not well visualized for one 3D printed model and another surgeon had difficulty visualizing the base of the prostate due to its relationship with the bladder neck for one AR model. The pre-surgical planning surveys were completed for 7 patients (38.9%) with imaging only and all patients with 3D printed and AR models. For these patients with 3D printed or AR models, the survey was completed using imaging only before visualizing the model for 21 patients (87.5%); and these survey results showed changes in surgical plan for decisions regarding nerve sparing (n=8, 33.3%), positive margins (n=7, 29.2%), and potency (n=7, 29.2%). 3D printing/AR performed better than imaging with respect to questions on anatomical details, confidence regarding surgical plan, and needing more information to help with planning (p = 0.04, p=0.01, and p = 0.01 respectively). Furthermore, there were significant differences between the following: operative times with 3D printed models as compared to imaging only (206 ± 14 mins, 233 ± 32 mins, p = 0.01), operative times for all 3D models compared to imaging only (210 ± 21 mins, 233 ± 32 mins, p = 0.04), and blood loss with AR models as compared to imaging alone (181 ± 93 mL, 258 ± 116 mL, p = 0.04). Figure 4 shows summary quantitative data for all patients stratified by surgeon.Discussion/Conclusion
In this study, we performed an initial evaluation on the impact that 3D printed and AR models can have on pre-surgical planning decisions as well as quantitative metrics including blood loss and operative times. Our initial results suggest that 3D models (both 3D printed and AR) demonstrate better anatomical details as per surgeons and improve their confidence in the surgical plan. Furthermore, in this initial evaluation, pre-operative patient-specific 3D printed and AR prostate cancer models reduced blood loss and operative times in patients undergoing robotic prostatectomy.Acknowledgements
This work was supported by the Center for Advanced Imaging Innovation and Research (www.cai2r.net), a NIBIB Biomedical Technology Resource Center (NIH P41 EB017183). In-kind support for this project from Stratasys.References
1. Wake N, Chandarana H, Huang WC, Taneja SS, Rosenkrantz AB. Application of anatomically accurate, patient-specific 3D printed models from MRI data in urological oncology. Clin Rad. 71(6) June 2016, p610-614.
2. Wake N, Rosenkrantz A, Ream J, Huang WC, Cohen S, Taneja SS, Sodickson DK, Chandarana H. Creation and Application of 3D Augmented Reality Cancer Models for Use in Abdominal Surgery. Radiological Society of North America. November 2017.
Figures
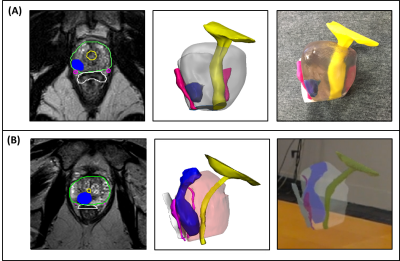
Figure 1: A) Image segmentation (left), 3D computer model (center), and 3D printed model (right) for one subject. B) Image segmentation (left), 3D computer model (center), and AR model (right) for another subject.
Dominant lesion –blue, prostate – (clear/pink on 3D, green on segmentation), rectal wall –white, bladder/urethra – yellow, nerves –dark pink.