0713
Four-dimensional T2-weighted imaging in prostate MRI with T2 shuffling1Radiology, Stanford University, Stanford, CA, United States, 2Electrical Engineering and Computer Sciences, University of California, Berkeley, Berkeley, CA, United States, 3Applications and Workflow, GE Healthcare, Menlo Park, CA, United States
Synopsis
High-quality T2-weighted imaging is critical in the evaluation of the prostatic transition zone for cancer. We adapted an acquisition technique currently used mostly in musculoskeletal MRI termed T2 Shuffling (T2Sh) by incorporating outer volume suppression (OVS) and optimizing it for the prostate. Our retrospective review of 20 patients assessed T2Sh in the evaluation of the prostate. The overall image quality of T2Sh was comparable to that of 2D T2 FSE with water-fat separation and superior to that of 3D T2 FSE with OVS and water-fat separation.
Introduction
Prostate Imaging Reporting And Data System (PI-RADS) version 2 assigns T2-weighted imaging (T2) as the dominant score for assessing lesions in the transition zone, the location of approximately 20-30% of prostate cancers [1]. Due to Benign Prostatic Hyperplasia (BPH), evaluation of the transition zone can be challenging, making high-quality T2-weighted imaging critical to accurate assessment [2-6].
This study evaluates a redesigned volumetric Fast Spin Echo (FSE) sequence with variable refocusing flip angles that resamples k-space positions at multiple echo times (TE), effectively supporting a four-dimensional reconstruction of images varying from Proton Density (PD) to heavy T2 weighting [7]. We hypothesize that this technique, termed T2 Shuffling (T2Sh), combined with outer volume suppression (OVS) [8], is feasible and may be superior to standard 2D and 3D T2 sequences in the evaluation of the prostate.
Methods
3D FSE sequence (CUBE) was redesigned to randomly shuffle and re-acquire phase encodes during each echo train [7]. To optimize T2Sh for the prostate, we incorporated OVS to significantly reduce the effective field of view [9] (Figure 1). Data reconstruction used locally low rank regularization to exploit volumetric redundancy [7].
Twenty consecutive patients who underwent prostate MRI with 2D axial T2 FSE with water-fat separation (2D FSE-Flex), a 3D T2 FSE with OVS and water-fat separation (CUBE-Flex), and T2Sh with OVS and fat suppression (Table 1) were retrospectively identified. Note 2D FSE-Flex and CUBE-Flex provide both fat-suppressed and conventional non-fat-suppressed images, and fat suppression was applied to T2Sh for better prostate visualization [9]. T2 maps of the prostate region were computed based on the extended phase graph formalism with non-linear least-squares, but was not used for evaluation.
Three radiologists performed blinded and independent evaluations on a Likert scale of each fat-suppressed T2 sequence in the axial plane (2D FSE-Flex, CUBE-Flex, and T2Sh reconstructed at an equivalent TE of 100 ms [10]) for image quality, anatomic delineation, and diagnostic confidence. Subsequently, the three sequences were reevaluated for overall image quality and directly compared to each other with simultaneous viewing.
Comparison of the three sequences was performed with one-way ANalysis Of VAriance (ANOVA), post-hoc Tukey Honestly Significant Difference (HSD) test, and Bonferroni-Holm correction for multiple comparisons. Inter-observer agreement was evaluated with Intraclass Correlation Coefficients (ICC).
Results
The mean age of our patients was 66 years, with mean Prostate-Specific Antigen (PSA) level of 10.9 ng/mL. Of our 20 patients, six had no prostate lesions (30%). The remaining 14 patients had 17 lesions, five of which located in the transition zone (29%). End-to-end (raw data to DICOM) reconstruction time was 10 minutes on a 24-core Xeon E5-2670 machine.
T2Sh demonstrated better contrast than both 2D FSE-Flex and CUBE-Flex (p = 0.0015). Otherwise, there was no statistical difference between T2Sh and 2D FSE-Flex in image quality, anatomic delineation, and diagnostic confidence, although both T2Sh and 2D FSE-Flex performed better than CUBE-Flex in all image quality features (Table 2). Direct paired comparisons of overall image quality of the three sequences demonstrated similar results: the readers preferred both T2Sh and 2D FSE-Flex more than CUBE-Flex, while T2Sh and 2D FSE-Flex rated similarly with a slight trend favoring T2Sh (Table 3). Inter-observer agreement was greater overall for 2D FSE-Flex and CUBE-Flex than T2Sh, possibly due to reader unfamiliarity with T2Sh. 2D FSE-Flex and CUBE-Flex had five and six (out of nine) parameters, respectively, with good to excellent inter-observer agreement (ICC > 0.60), compared to T2Sh with three (Table 2).
Discussion
Overall, T2Sh was comparable to 2D FSE-Flex and superior to CUBE-Flex in the evaluation of the prostate. This level of performance did not factor in additional potential advantages of T2Sh, including T2 mapping and retrospectively varying T2 weighting afforded by resampling at multiple TEs, and multiplanar reconstructions from volumetric acquisition.
The value of T2 mapping in the prostate was not assessed in our study. Current uses of T2 mapping predominate in musculoskeletal MRI, a natural application since protocols rely on multiplanar PD and T2-weighted imaging, which all can be acquired with T2Sh [11]. Potential benefits of T2 mapping in the prostate include quantitative T2 values of transition-zone cancers (Figure 2). The disadvantages of T2Sh include its longer scan and reconstruction times. If T2 mapping and multiplanar reformatting can improve prostate cancer detection, this advantage would outweigh the increased scan and reconstruction times.
Conclusion
T2Sh in the prostate is feasible and yields image quality comparable to 2D FSE-Flex and superior to CUBE-Flex. T2 mapping from T2Sh has further potential to improve prostate cancer detection in the transition zone, a question that requires further study.Acknowledgements
This work is supported by NIBIB R01EB009690 and GE Healthcare.References
1. Weinreb JC, Barentsz JO, et al. PI-RADS Prostate Imaging-Reporting and Data System: 2015, Version 2. Eur Urol 2016; 69: 16-40.
2. Gupta RT, Spilseth B, et al. Multiparametric prostate MRI: focus on T2-weighted imaging and role in staging of prostate cancer. Abdom Radiol 2016; 41: 831-843.
3. Greer MD, Shih JH, et al. Validation of the dominant sequence paradigm and role of dynamic contrast-enhanced imaging in PI-RADS version 2. Radiology 2017; 286(1): 1-11.
4. Rosenkrantz AB, Neil J, et al. Prostate cancer: comparison of 3D T2-weighted with conventional T2-weighted imaging for image quality and tumor detection. Am J Roentgenol 2010; 194: 446-452.
5. Itatani R, Namimoto, et al. Extracapsular extension of prostate cancer: diagnostic value of combined multiparametric magnetic resonance imaging and isovoxel 3-dimensional T2-weighted imaging at 1.5 T. J Comput Assist Tomogr 2015; 39(1): 37-43.
6. Tanaka U, Ueno Y, et al. Value of three-dimensional T2-weighted turbo spin-echo imaging with tissue-specific variable refocusing flip angle for 3-T magnetic resonance imaging of prostate cancer: comparison with conventional two- and three-dimensional T2-weighted turbo spin-echo imaging. Jpn J Radiol 2017; https://doi.org/10.1007/s11604-017-0684-1.
7. Tamir JI, Uecker M, et al. T2 shuffling: sharp, multicontrast, volumetric fast spin-echo imaging. MRM 2016; 77: 180-195.
8. Stoddard PB, Taviani V, et al. 3D T2-weighted fast spin echo (FSE) with outer volume suppression versus 2D FSE in the prostate: comparison of lesion detection in the transition zone and image quality. Proc ISMRM 2017, 2092.
9. Han M, Chiba K, et al. Variable flip angle 3D fast spin-echo sequence combined with outer volume suppression for imaging trabecular bone structure of the proximal femur. J Magn Reson Imaging. 2015; 41: 1300-1310.
10. Busse RF, Hariharan H, et al. Fast spin echo sequences with very long echo trains: design of variable refocusing flip angle schedules and generation of clinical T2 contrast. MRM 2006; 55: 1030-1037.
11. Bao S, Tamir JI, et al. Fast comprehensive single-sequence four-dimensional pediatric knee MRI with T2 shuffling. J Magn Reson Imaging 2017; 45: 1700-1711.
12. Flood TF, Pokharel SS, et al. Accuracy and interobserver variability in reporting of PI-RADS version 2. JACR 2017; 14(9): 1202-1205.
Figures
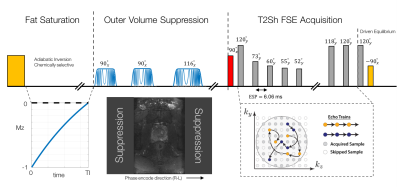
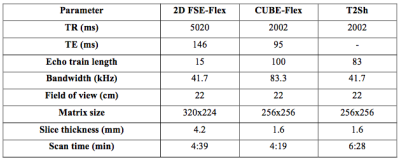
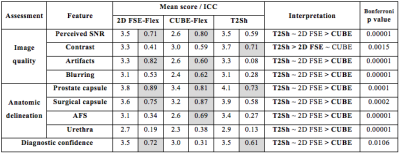
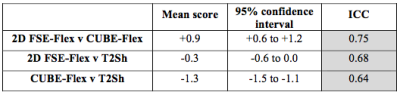
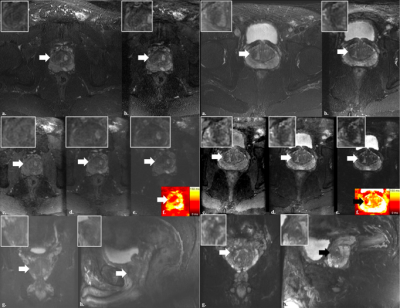
Figure 2: Two representative cases with transition zone prostate lesions labeled on each sequence with white/black arrows. Note the increasing conspicuity of the lesions with increasing echo times (TE) in T2Sh.
a. 2D FSE-Flex; b. CUBE-Flex; c-e. T2Sh reconstructed at equivalent TE of 20 ms, 100 ms, and 200 ms, respectively; f. T2 map from T2Sh; g. coronal reconstruction of T2Sh at equivalent TE of 100 ms; h. sagittal reconstruction of T2Sh at equivalent TE of 100 ms.